Emergency Medicine 7
Session: Emergency Medicine 7
093 - Comparative Effectiveness of 1 Versus 2 Doses of Dexamethasone for Pediatric Asthma Exacerbations
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 93.4352
Shivam Dave, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Daniel Shapiro, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Israel Green-Hopkins, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States

Shivam Dave, MD (he/him/his)
PGY-2
UCSF Benioff Children's Hospital San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: In children with asthma exacerbations managed as outpatients, treatment with 1-2 doses of dexamethasone is noninferior to 3-5 days of prednisone, with fewer adverse effects and improved adherence. However, whether children treated with 1 dose of dexamethasone have different outcomes from those treated with 2 doses is uncertain. Determining the minimum effective duration of corticosteroid therapy is critical in reducing the harms and costs of overtreatment.
Objective: To compare effectiveness of 1 vs. 2 doses of dexamethasone for children with asthma exacerbations discharged from the emergency department (ED).
Design/Methods: This was a retrospective (2017-2024) cohort study of children, ages 2-20 years, diagnosed with asthma (ICD-10=J45.X), discharged from 1 of 2 pediatric EDs, who received dexamethasone in the ED. Exclusion criteria were an ED visit or hospitalization in the previous 14 days, treatment with systemic corticosteroids in the previous 7 days, treatment with corticosteroids other than dexamethasone at the visit, or co-diagnosis of a condition warranting corticosteroids. The primary outcome was an ED revisit, and the secondary outcomes were hospitalization or new treatment with systemic corticosteroids, all assessed 1-14 days after the index visit. The primary exposure was whether a 2nd dexamethasone dose was prescribed at discharge. To adjust for baseline differences across exposure groups in the comparative effectiveness analysis, we generated propensity scores and used inverse probability weighted logistic regression.
Results: Among 1,635 patients included, the median age was 5 years (IQR: 3-7 years), and 62.9% were male (Table 1). Overall, 609 (37.2%) received 1 dose of dexamethasone, and 1,026 (62.8%) received 2 doses. In the propensity score-weighted analysis, the adjusted risk of an ED revisit was 7.3% (95% CI: 5.9-9.7%) for patients who received 1 dose of dexamethasone and 7.6% (95% CI: 5.9-9.2%) for those who received 2 doses (risk difference: 0.21%, 95% CI: -2.6% to 3.0%). The risks of hospitalization and new corticosteroid treatment during the follow-up period did not differ across exposure groups (Table 2).
Conclusion(s): Nearly two thirds of children discharged from the ED after asthma exacerbations were treated with 2 doses of dexamethasone, but risks of ED revisits, hospitalizations, and new corticosteroid treatment did not differ based on whether 1 or 2 dexamethasone doses were used. These findings suggest that 1 dose of dexamethasone may be sufficient for many children and highlight the importance of future studies to identify these children.
Table 1. Characteristics of children with asthma exacerbations included in the cohort
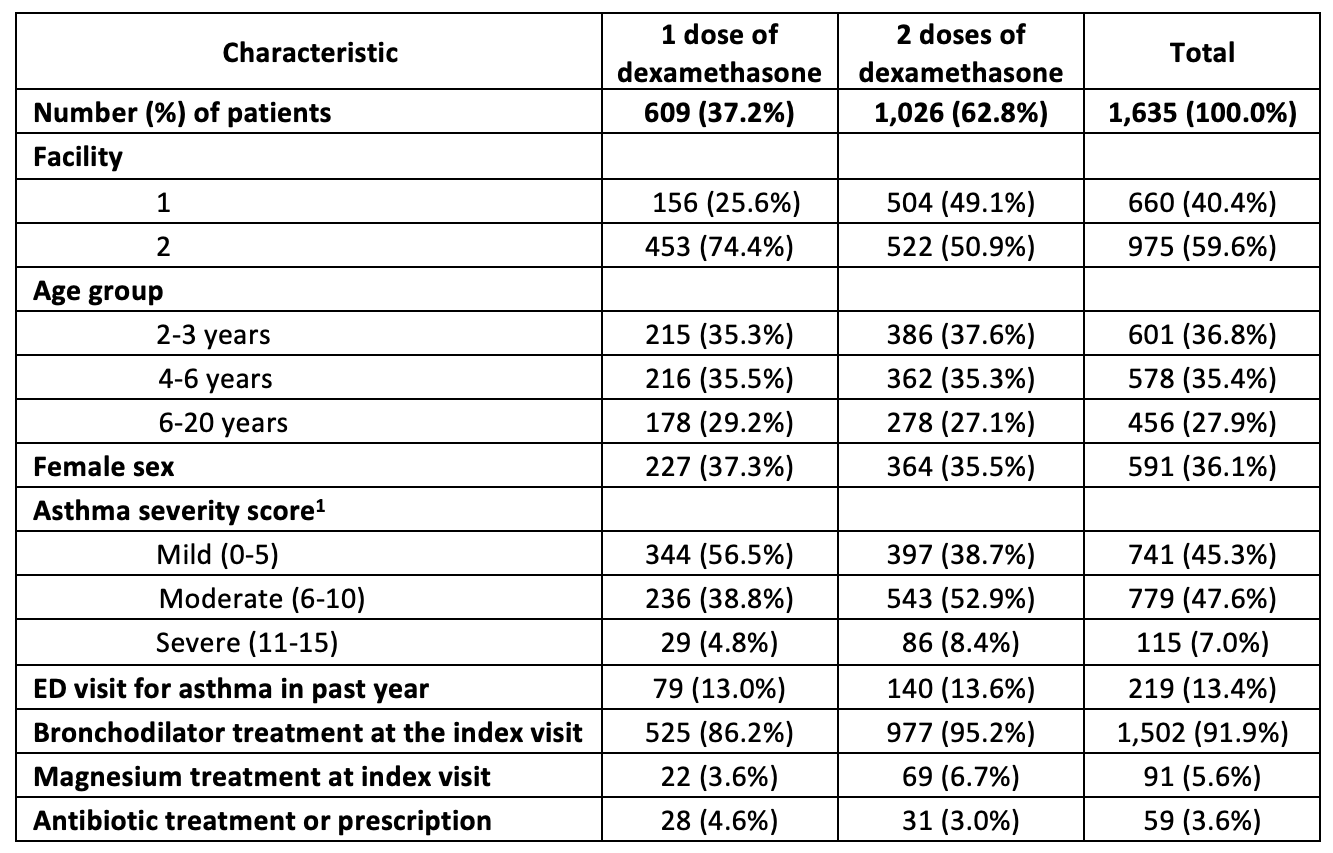 1. Based on the Modified Pediatric Asthma Severity Score, a standardized scoring system used at both facilities in this study.
1. Based on the Modified Pediatric Asthma Severity Score, a standardized scoring system used at both facilities in this study.Table 2. Risks of emergency department revisits, hospitalizations, and new corticosteroid treatments during the 14-day follow-up period
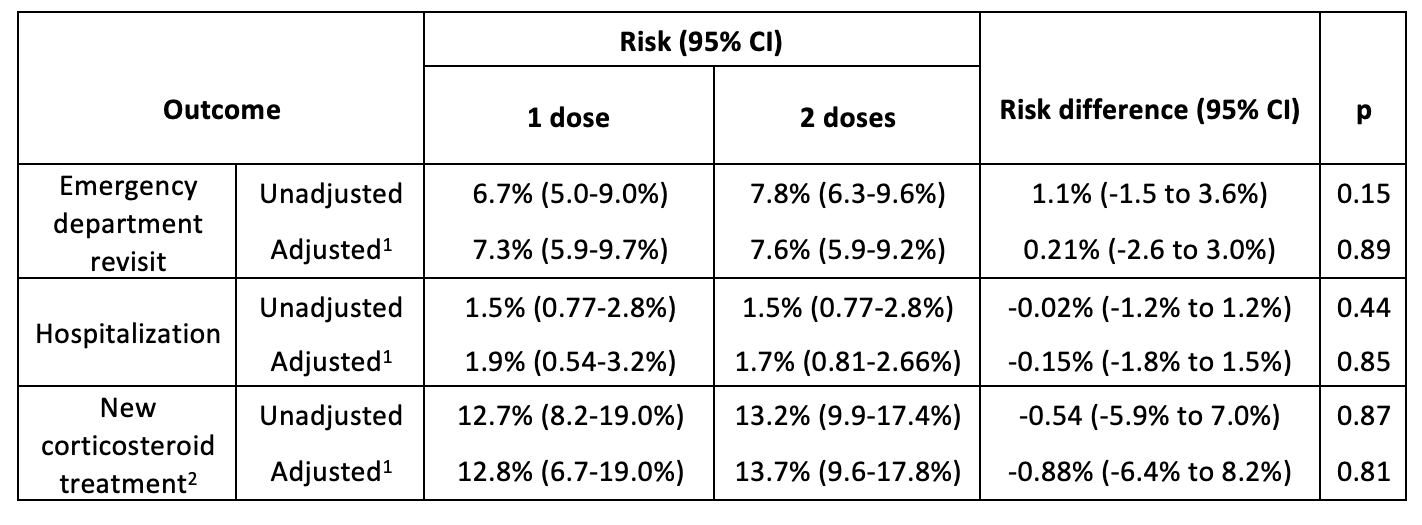 1. Adjusted risks and risks differences are from a logistic regression model weighted by the inverse probability of treatment with a second dose of dexamethasone. Propensity scores were determined by logistic regression with dexamethasone treatment (1 vs. 2 doses) as the outcome. We included the following covariates: year, facility, age, asthma severity score, prior emergency department visits for asthma, and other treatments (e.g., magnesium) at the index visit.
1. Adjusted risks and risks differences are from a logistic regression model weighted by the inverse probability of treatment with a second dose of dexamethasone. Propensity scores were determined by logistic regression with dexamethasone treatment (1 vs. 2 doses) as the outcome. We included the following covariates: year, facility, age, asthma severity score, prior emergency department visits for asthma, and other treatments (e.g., magnesium) at the index visit. 2. The risk of a new corticosteroid treatment was calculated only for children who received primary care within the emergency departments’ healthcare system, as outpatient care for other children would not be captured in the electronic health record.

