Children with Chronic Conditions 1
Session: Children with Chronic Conditions 1
493 - Connecting the Fragments: A Comprehensive Quality Improvement Initiative to Enhance Safety and Optimize Throughput for Children with Medical Complexity
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 493.4539
Wendy Arafiles, Phoenix Children's, Phoenix, AZ, United States; Hannah Challa, Phoenix Children's Hospital, Phoenix, AZ, United States

Wendy Arafiles, MD, FAAP (she/her/hers)
Assistant Clinical Professor
Phoenix Children's
Phoenix, Arizona, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) experience fragmented healthcare resulting in high resource utilization. CMC spend a disproportionate amount of time in the inpatient care setting with high average lengths of stay and high readmission rates. Individual pediatric institutions are challenged to design programs that streamline concurrent inpatient care and care transitions for a heterogeneous population within tight financial margins.
Objective: Over two years, the hospital medicine division at a freestanding children’s hospital focused on enhancing inpatient continuity of care for a subpopulation of the institution’s CMC. A series of interventions funded through both charitable contribution and capital investment were implemented to optimize communication, close care gaps, and improve inpatient throughput.
Design/Methods: Initial interventions included the appointment of a Medical Director of Complex Care to utilize resourceful problem-solving and create change strategies. After securing funding and onboarding team members, quality improvement methods were employed to implement and study interventions outlined in Table 1. Process, outcome, and balancing measures for both inpatient throughput and patient/caregiver communication were recorded on run charts. Outcomes were presented to various audiences in clinical, safety and quality, revenue cycle, and leadership sectors of the institution.
Results: Compared to the pre-implementation year of 2021, the series of interventions over 2022 and 2023 yielded an 18% decrease in average median length of stay (Figure 1), 41% decrease in average 7-day and 30% decrease in average 30-day unplanned readmission rates (Figure 2), despite a 5% increase in complexity and 38% increase in volume (Figure 1). The inpatient Complex Care Program yielded 99% attempt and 82% connect rates for post-discharge follow up phone calls; 37% of the connected calls resulted in mitigative action for issues with prescriptions, home health orders, documentation, and care advice.
Conclusion(s): In the inpatient environment, CMC benefit from enhanced continuity of care providers and intentional care coordination. Skilled post-discharge follow-up communication facilitates timely mitigation of issues and gap coverage. The positive trend of measures in this comprehensive quality improvement initiative suggests that a small team of dedicated providers and staff can sustainably create impactful change that benefits patients and their caregivers as well as the institution.
Table 1. Inpatient Interventions to Improve Safety and Throughput for CMC
.png) Interventions implemented over the two calendar years of the initiative to improve quality and efficiency of care for CMC.
Interventions implemented over the two calendar years of the initiative to improve quality and efficiency of care for CMC.Figure 1: Median length of stay, Case Mix Index (CMI), and volume of a subpopulation of CMC discharged by Hospital Medicine cohort.
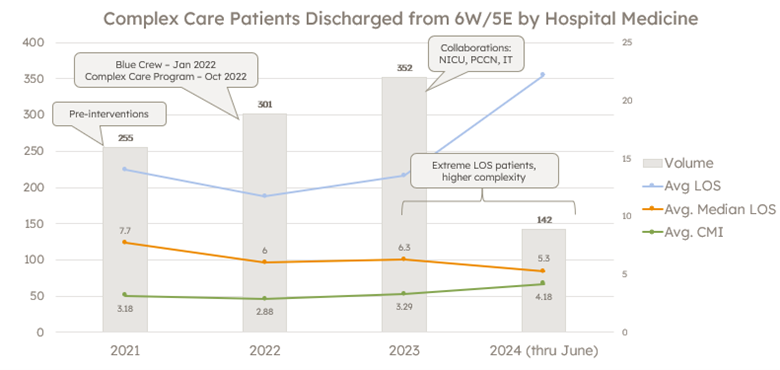 Year over year measures for volume of CMC discharged by Hospital Medicine from the inpatient unit designated for the cohort population of CMC with home invasive ventilation. LOS = length of stay; CMI = case mix index.
Year over year measures for volume of CMC discharged by Hospital Medicine from the inpatient unit designated for the cohort population of CMC with home invasive ventilation. LOS = length of stay; CMI = case mix index.Figure 2: 7- and 30-day unplanned readmission rate with volume of a subpopulation of CMC discharged by Hospital Medicine cohort.
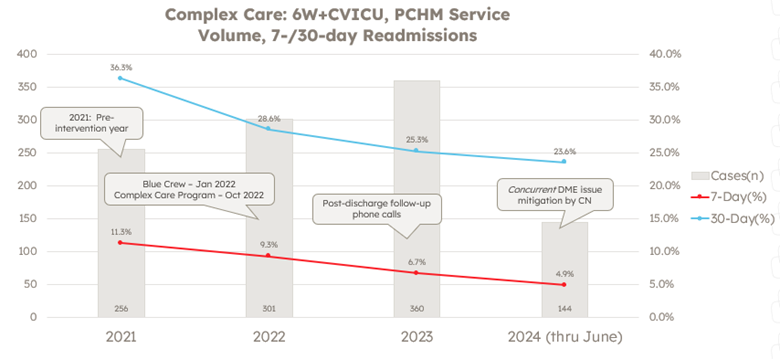 Year over year measures for 7- and 30-day unplanned readmission rates and volume of CMC discharged by Hospital Medicine from the inpatient unit designated for the cohort population of CMC with home invasive ventilation. DME = durable medical equipment; CN = care navigator
Year over year measures for 7- and 30-day unplanned readmission rates and volume of CMC discharged by Hospital Medicine from the inpatient unit designated for the cohort population of CMC with home invasive ventilation. DME = durable medical equipment; CN = care navigator
