Child Abuse & Neglect 2
Session: Child Abuse & Neglect 2
350 - Adverse Childhood Experiences Screening and Pediatric Developmental Screening in Primary Care Patients in Los Angeles
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 350.3725
Morgan Ye, University of California, San Francisco, School of Medicine, Dublin, CA, United States; India Gill, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Andrew V. Nguyen, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Celia Draycott, ACEs-LA, Los Angeles County Health Services, Brooklyn, NY, United States; Nina N. Thompson, Olive View-UCLA Education and Research Institute, San Francisco, CA, United States; Amy Shekarchi, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Danielle Hessler Jones, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Dayna Long, UCSF Benioff Children's Hospital Oakland, Oaklnad, CA, United States; Matthew S. Pantell, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Neeta Thakur, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Edward Machtinger, University of California, San Francisco, San Francisco, CA, United States; Shannon M.. Thyne, David Geffen School of Medicine at UCLA, SYLMAR, CA, United States
- MY
Morgan Ye, MPH (she/her/hers)
Research Data Analyst
University of California, San Francisco, School of Medicine
Dublin, California, United States
Presenting Author(s)
Background: Evidence shows that adverse childhood experiences (ACEs) are associated with child developmental delays. Although the American Academy of Pediatrics has recommended screening for childhood adversity, there is a limited understanding of the impacts of introducing standardized prospective ACE screening as part of healthcare on clinical developmental metrics.
Objective: The objective of this study was to assess the association between ACE screening and achievement of pediatric developmental screening in primary care patients in Los Angeles.
Design/Methods: We queried 2020 to 2023 electronic health record (EHR) data from children aged 0-18 years who visited 10 primary care clinics that are part of the Los Angeles County Department of Health Services. ACE screening status was based on the completion of the 10 ACEs items in the PEdiatric ACEs and Related Life Event Screener (PEARLS). Pediatric developmental metrics, including completion of developmental assessment (Ages & Stages Questionnaires-3 (ASQ-3) at 9, 18, and 30 months), autism screening (Modified Checklist for Autism in Toddlers (M-CHAT) before 30 months), and well-child visits was obtained from the EHR wellness registries. Multivariable logistic regressions were used to assess the association between ACE screening and pediatric developmental metrics. Models were propensity score matched on child age, gender, insurance, clinic, appointment type, number of primary care visits, and primary care visit date quartile. Outcome models were further adjusted on covariates if standardized mean differences were greater than 0.2.
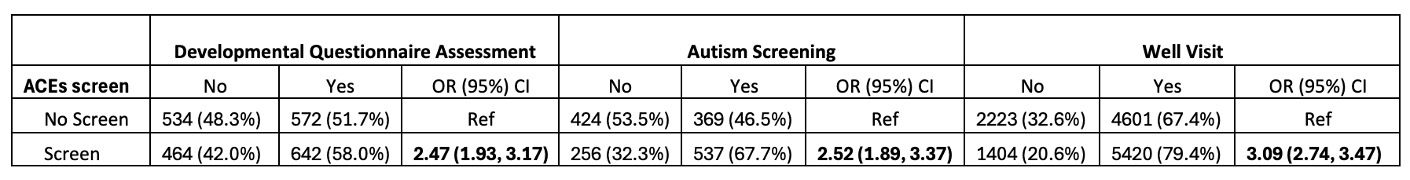
Results: In our matched dataset, the achievement rates were 55%, 57%, and 73% for developmental assessment (n=2212), autism screening (n=1586), and well-child visits (n=13648), respectively. Children who were screened for ACEs were more likely to achieve screenings for developmental assessment (odds ratio (OR) 2.47; 95% CI: 1.93, 3.17) and autism (OR 2.52; 95% CI: 1.89, 3.37) compared to those not screened for ACEs. ACE screening was also significantly associated with increased odds of having a well-child visit (OR 3.09; 95% CI: 2.74, 3.47).
Conclusion(s): In a pediatric primary care patient population, we found that ACE screening was associated with increased achievement of pediatric developmental metrics. These results emphasize the importance of ACE screening in preventing and reducing adverse outcome in child development and expediting patients’ access to services and referrals to resources.
Association between ACE screening and pediatric developmental metrics