Emergency Medicine 8
Session: Emergency Medicine 8
108 - Asthma Risk in Children Treated with High-Flow Nasal Cannula for Bronchiolitis: A Retrospective Cohort Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 108.3595
Andrea Rivera-Sepulveda, Nemours Children’s Health, Orlando, FL, United States; Lindsey Ammann, University of Central Florida College of Medicine, Orlando, FL, United States; Arielle Hough, Nemours Children's Hospital, Orlando, FL, United States; Sophia G. Blumenfeld, Mayo Clinic Alix School of Medicine, Ponte Vedra Beach, FL, United States; Zhuo Li, Mayo Clinic Alix School of Medicine, jacksonville, FL, United States; Matthew M. Davis, Nemours Children's Hospital, Wilmington, DE, United States

Lindsey Ammann (she/her/hers)
Medical Student
University of Central Florida College of Medicine
Orlando, Florida, United States
Presenting Author(s)
Background: High-flow nasal cannula (HFNC) is a common intervention for children with moderate to severe bronchiolitis. Studies suggest that severe bronchiolitis in early childhood, particularly cases requiring hospitalization, is associated with an increased risk of asthma later in life. Additionally, using HFNC during a bronchiolitis episode may indicate a more severe disease, raising concerns about long-term respiratory issues like asthma. The effects of pressure-derived non-invasive ventilatory (NIV) support and the impact of HFNC in children with bronchiolitis who develop asthma are underexplored.
Objective: This study aims to examine the association between HFNC use in the management of bronchiolitis and the subsequent risk of developing asthma. We hypothesize that children with bronchiolitis who undergo HFNC have a higher prevalence of asthma later in life than children with bronchiolitis who do not undergo HFNC.
Design/Methods: This retrospective cohort study analyzed data from a large cohort of children with bronchiolitis treated with and without HFNC to serve as a predictive factor for asthma development from 2015-2023. Data included demographics, HFNC characteristics, time to asthma diagnosis, and cumulative episodes of bronchiolitis. Groups were compared using Wilcoxon rank sum test, and the chi-squared test, as indicated. Logistic regression analysis associated HFNC use in children with bronchiolitis and asthma.
Results: We identified 4736 children with bronchiolitis, of which 42.6% received HFNC. Of the 28% of patients who developed asthma, 55.7% underwent HFNC. Asthma risk was higher in children with bronchiolitis who used HFNC (OR 2.1, 95% CI 1.9-2.4), had longer HFNC duration (OR 2.5, 95% CI 2.1-3.1), human rhinovirus/enterovirus infection (OR 2.7, 95% CI 2.1-3.6), and bronchiolitis episodes (OR 1.5, 95% CI 1.4-1.5). The number of HFNC usage, respiratory syncytial virus infection, or emergency department acuity was not associated with a higher risk of asthma in children with bronchiolitis who used HFNC (p < 0.05).
Conclusion(s): HFNC treatment for children with bronchiolitis is associated with an increased risk of asthma within 3-5 years. Patients treated with HFNC had significantly higher asthma rates compared to those who did not receive HFNC. These results suggest that while HFNC is a common intervention, its long-term effects on respiratory health require further study. Understanding this relationship is critical for informing long-term clinical management and follow-up of children with severe bronchiolitis, potentially allowing for early intervention strategies to mitigate asthma risk.
Table 1
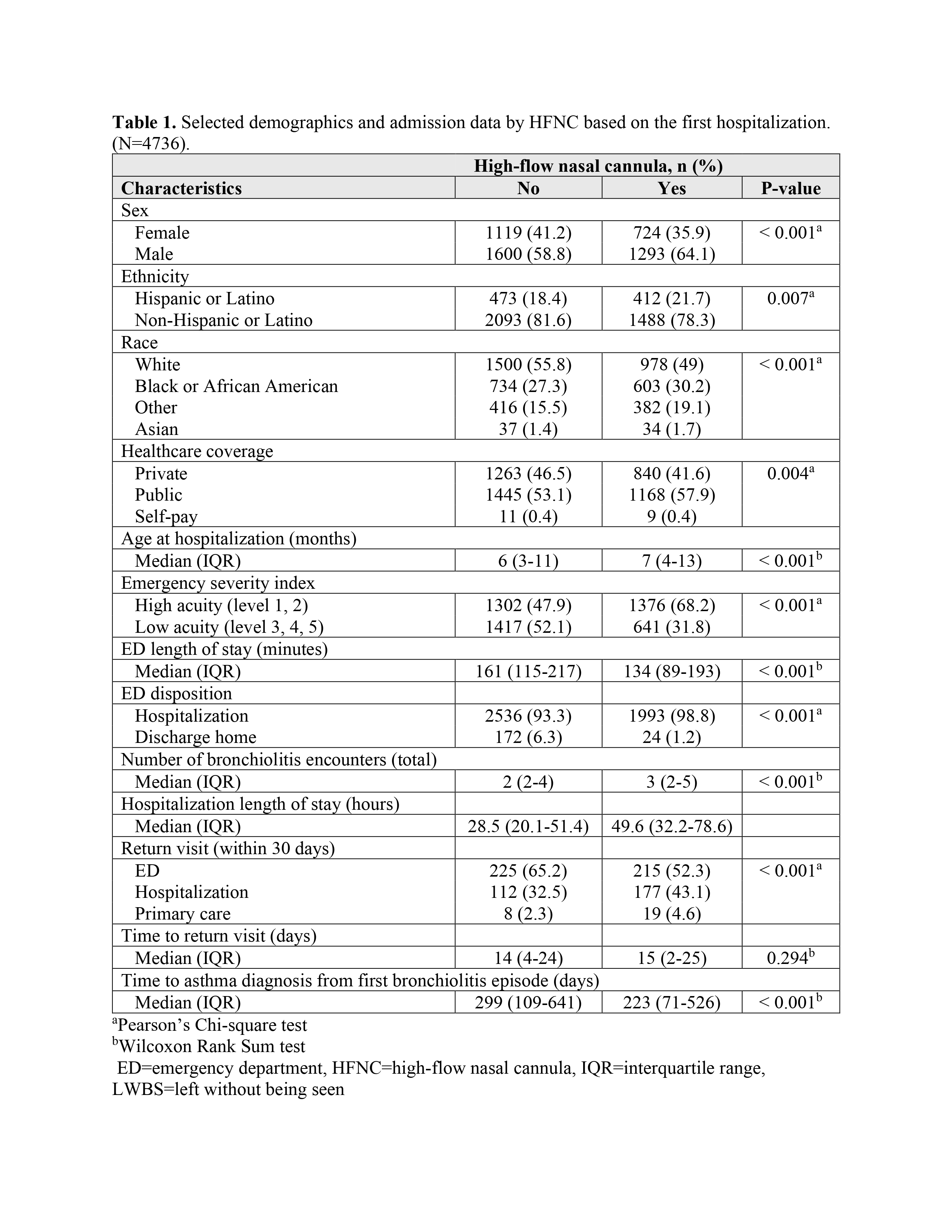 Selected demographics and admission data by HFNC based on the first hospitalization. (N=4736).
Selected demographics and admission data by HFNC based on the first hospitalization. (N=4736).Table 2
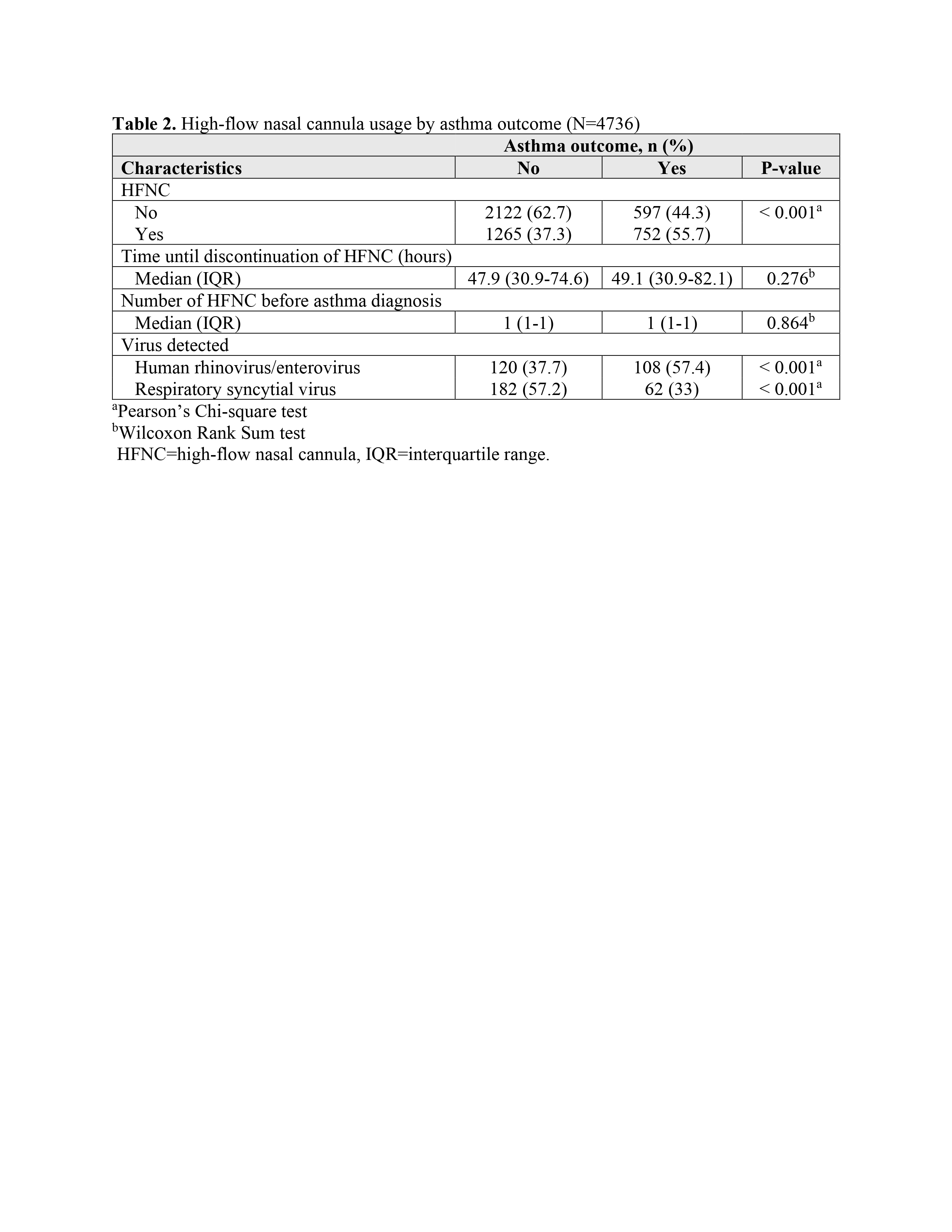 High-flow nasal cannula usage by asthma outcome (N=4736).
High-flow nasal cannula usage by asthma outcome (N=4736).Table 3
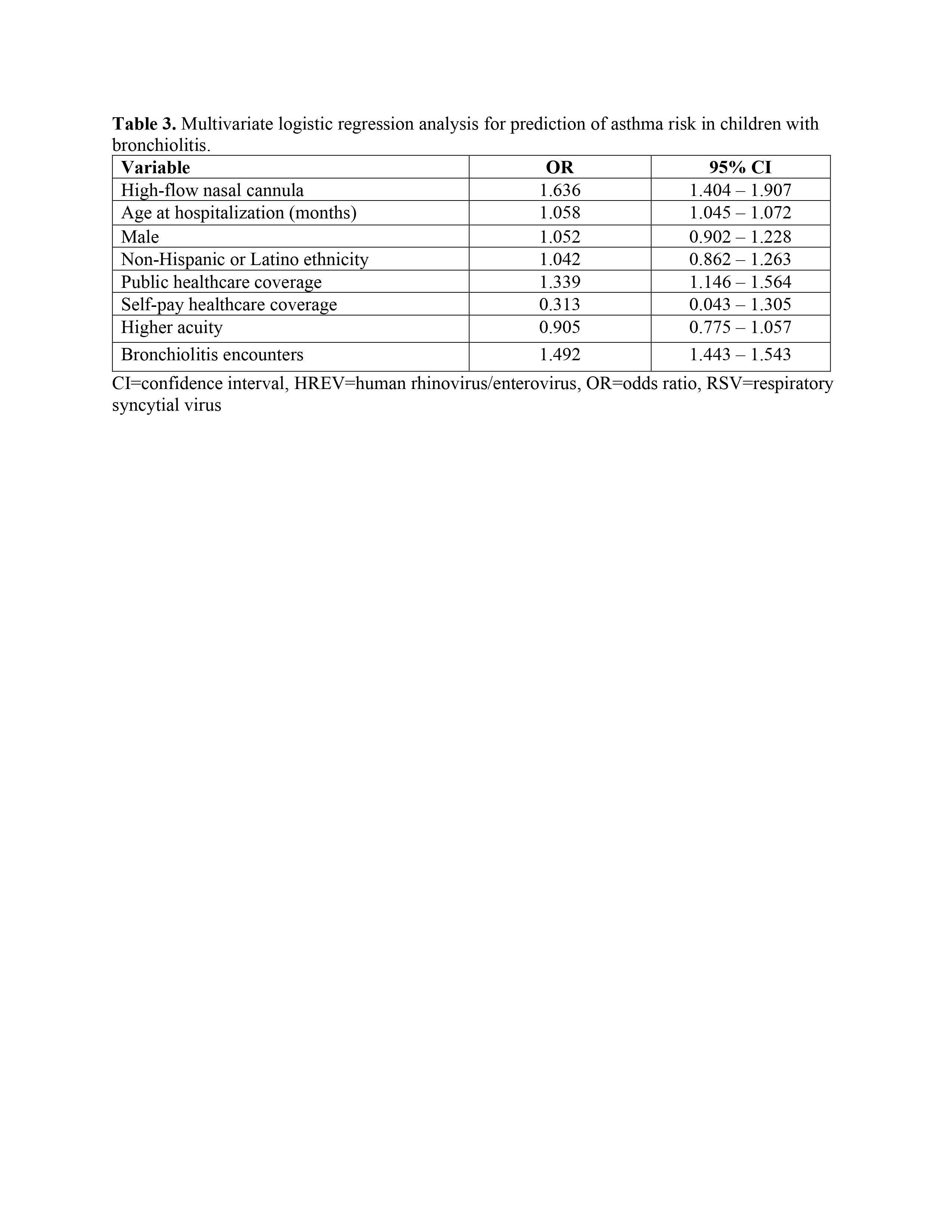 Multivariate logistic regression analysis for prediction of asthma risk in children with bronchiolitis.
Multivariate logistic regression analysis for prediction of asthma risk in children with bronchiolitis.Table 1
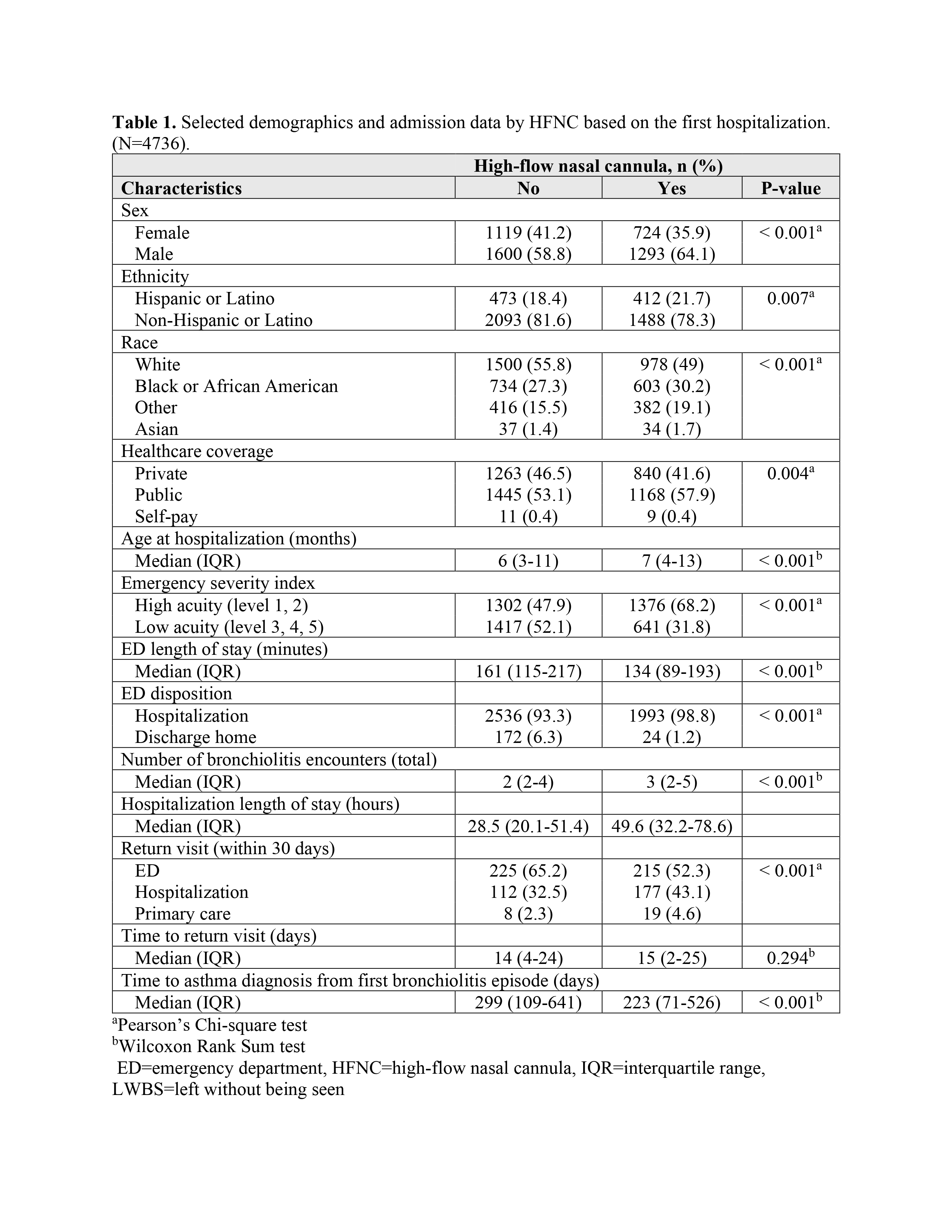 Selected demographics and admission data by HFNC based on the first hospitalization. (N=4736).
Selected demographics and admission data by HFNC based on the first hospitalization. (N=4736).Table 2
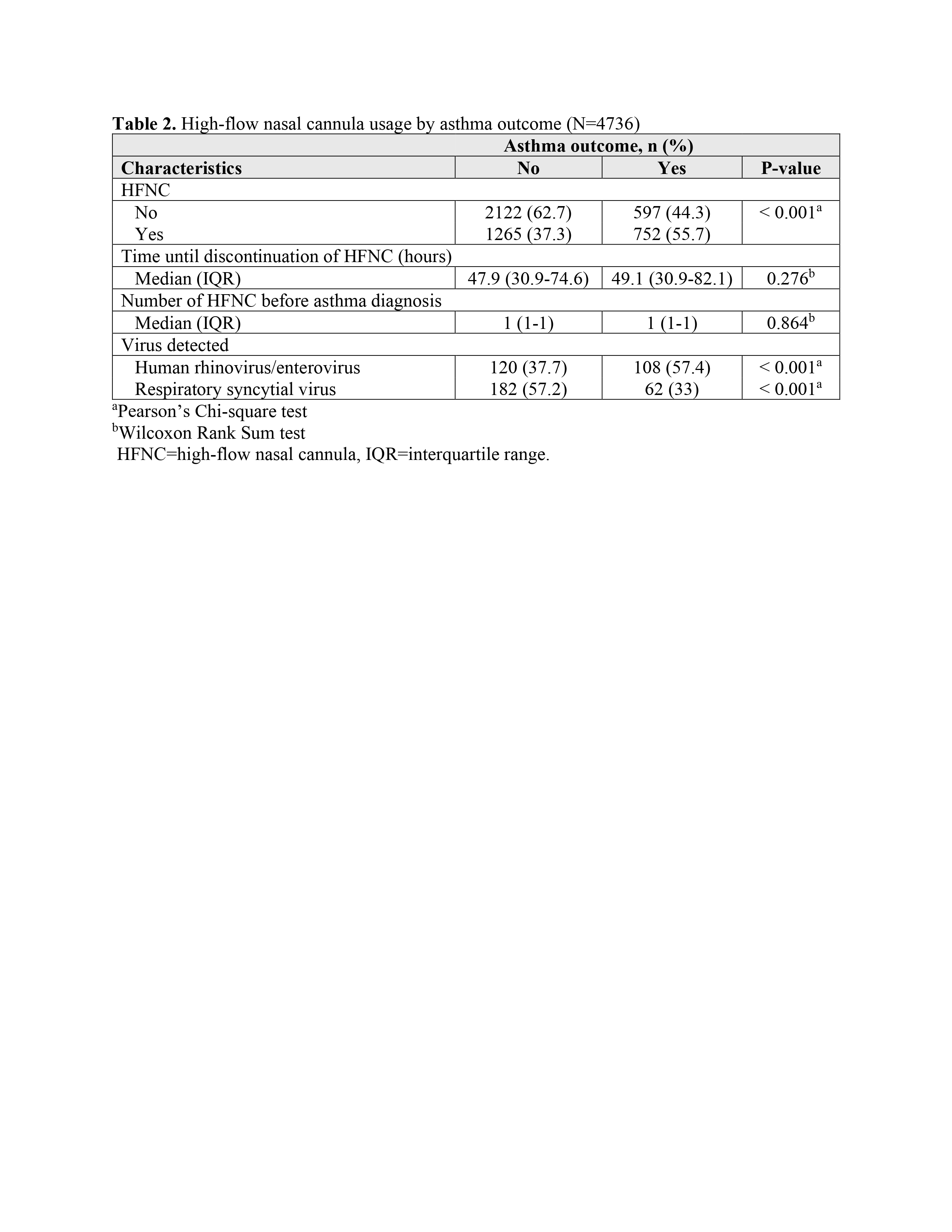 High-flow nasal cannula usage by asthma outcome (N=4736).
High-flow nasal cannula usage by asthma outcome (N=4736).Table 3
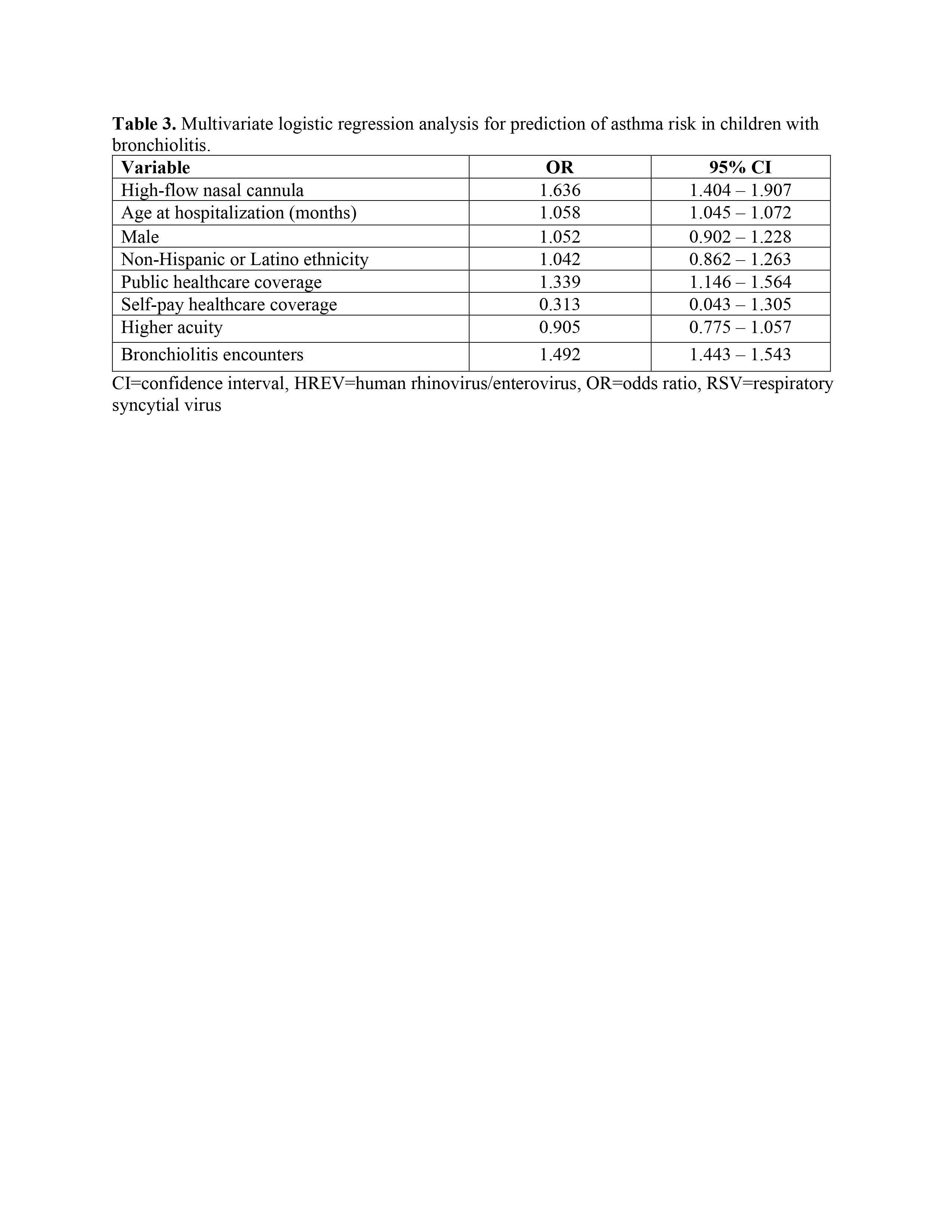 Multivariate logistic regression analysis for prediction of asthma risk in children with bronchiolitis.
Multivariate logistic regression analysis for prediction of asthma risk in children with bronchiolitis.
