Child Abuse & Neglect 2
Session: Child Abuse & Neglect 2
353 - Child Abuse Presenting as Growth Failure: A Case Series of Psychosocial Short Stature
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 353.4065
Mary Palmer, East Tn Children's Hospital, Knoxville, TN, United States; Suzanne Rybczynski, East Tennessee Children's Hospital, Knoxville, TN, United States; Elizabeth Wirthwein, East Tennessee Children’s Hospital, Knoxville, TN, United States

Mary Palmer, MD, FAAP (she/her/hers)
Child Abuse Pediatrician
East Tennessee Children's Hospital
Knoxville, Tennessee, United States
Presenting Author(s)
Background: Presentations to our institution of growth-stunted children from horrifically abusive settings revealed a paucity of current studies or review articles including psychosocial dysfunction as an etiology of growth failure. Our heightened awareness of this concern aided review of other patients and led to this clinical case series.
Objective: The aim of this study is to detail clinical features of growth failure and recovery seen with this type of abuse, thereby enhancing pediatric clinicians’ awareness of psychosocial short stature.
Design/Methods: This is a single-site retrospective case review study using descriptive statistics and exploratory nonparametric tests. Growth data were extracted for prior to entering the abusive setting, presentation for evaluation, and short ( < 1 year) and long (1-4year) term follow-up. Calculations for BMI, Height and Weight %-for-age, and Height Velocity were made using online calculators at Baylor Body Composition Laboratory (CDC growth charts) and Child Metrics (studies by Kelly et al and Baumgartner et al). Z scores (score of standard deviation from mean, SDS) allowed accurate comparison of data even in the extremes of growth failure. Non-parametric methods were used for analysis, including median values (M) and Wilcoxon Signed-Rank Test (at Social Science Statistics).
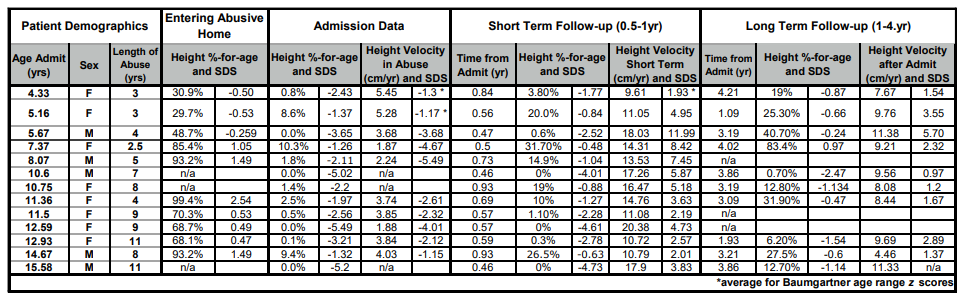
Results: Demographic, psychosocial and clinical features of 13 children are listed in Table 1. Growth data are presented in Tables 2 and 3. Weight & Height %-for-age SDS were significantly different after time in abusive setting (p <.01) suggesting that growth failure occurred in that environment (n=10). On admission all weighed less than 10%-for-age, however nutritional status ranged from normal to severe malnutrition using BMI-for-age SDS (0.11 to –7.03). BMI SDS varied in short (-1.32 to 2.04) and long-term (-1.28 to 2.56) follow up. Height %-for-age increased from a median of 0.8% on admission (range 0-10.3%) to 4% (range 0-31.7%) at < 1 year, and to 22% (0.7% to 83.4%) at 1-4yr. Height %-for-age SDS improvement from admission (M –2.43) to < 1yr follow up (M–1.77) was significant at p<.01. The median Height Velocity during abuse was 3.79 cm/yr (range 1.87-5.45, n=10), increasing to 14.31 cm/yr (9.61-20.38, n=13) at < 1yr. Height Velocity SDS increase from admission (M -2.47, n=10) to < 1yr (M4.18, n=10) was significant at p<.01.
Conclusion(s): Recognition of decreased growth velocity can be key to identifying psychosocial concerns ranging from simple family dysfunction to cruelty and torture. Intervention results in growth recovery on scale with treatment for other causes of short stature.
Table 1. Patient Demographics, Psychosocial and Clinical Features
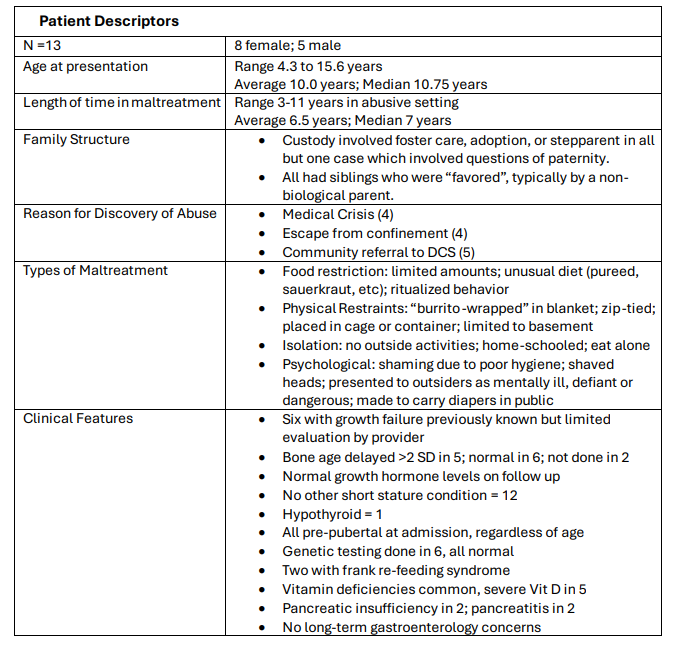
Table 2. Patient Weight %-for-age and BMI with z-scores
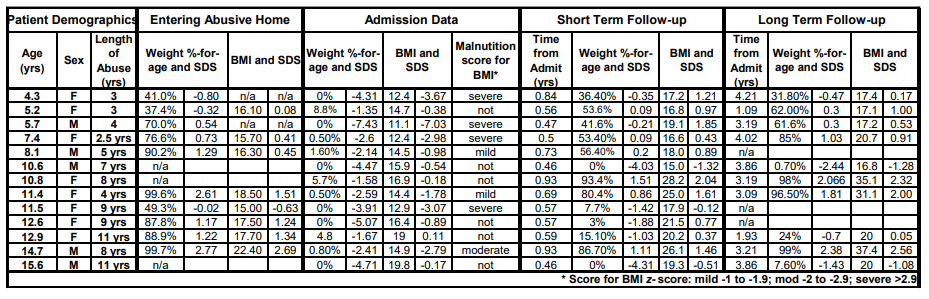
Table 3. Patient Height %-for-age and Height Velocity with z-scores
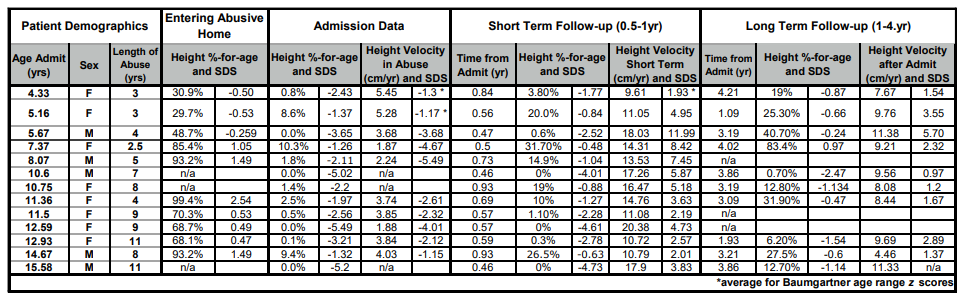
Table 1. Patient Demographics, Psychosocial and Clinical Features
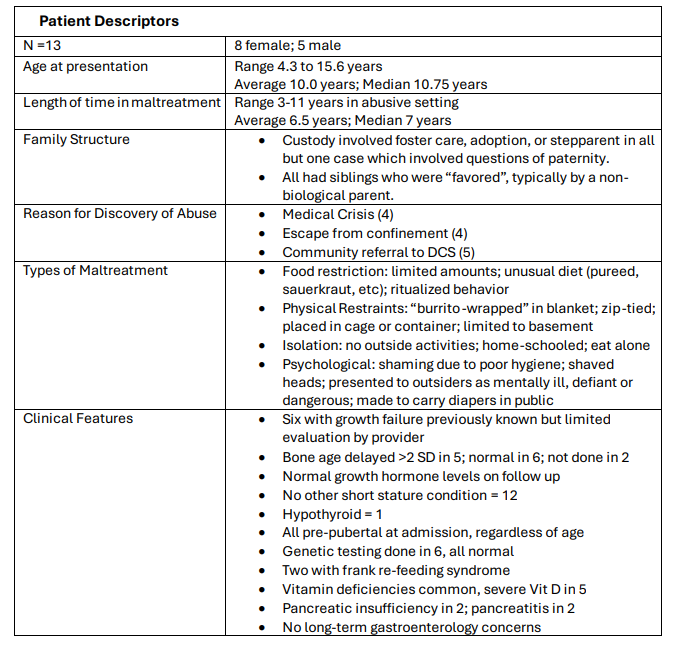
Table 2. Patient Weight %-for-age and BMI with z-scores
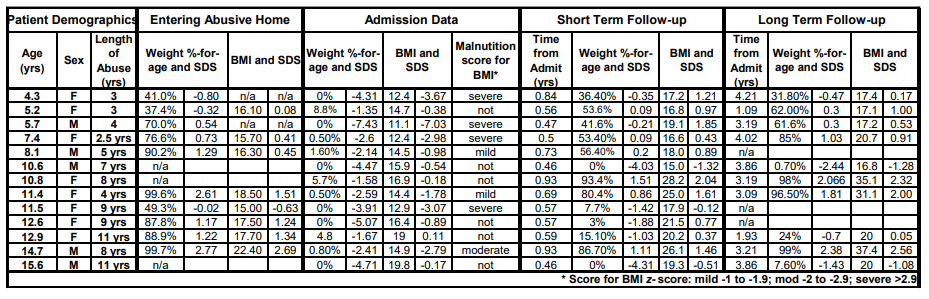
Table 3. Patient Height %-for-age and Height Velocity with z-scores