Global Neonatal & Children's Health 6
Session: Global Neonatal & Children's Health 6
796 - A Quality Improvement Project to Decrease CLABSI in Premature Neonates Admitted to a Level III NICU in Mauritius
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 796.3920
Shikha Sarkar, Connecticut Children's Medical Center, West Hartford, CT, United States; Muazzam Ally. Aumeer, Sir Anerood Jugnauth Hospital, Montagne blanche, Flacq, Mauritius; Oleg Miliavskyi, Sir Anerood Jugnauth Hospital, Brisee Verdiere, Flacq, Mauritius; Jacob Kelner, Connecticut Children's Medical Center, Hartford, CT, United States; Arvin Bundhoo, Connecticut Children’s Medical Center, Fairfield, CT, United States; Sunita Jugun, La Trobe University /Polytechnics Of Mauritius, Centre de Flacq, Flacq, Mauritius; Priya Ramessur, Central School of Nursing Mauritius, Flacq, Flacq, Mauritius; Pooja Soodun Boodhun, University of Mauritius, Riviere du Rempart, Riviere du Rempart, Mauritius; Hansinee Bissessur-Pursun, SAJ hospital, Flacq, Flacq, Mauritius; Logumbal Murugan, SSR Medical college, bon accueil, Flacq, Mauritius; Parakumaren Beemadoo, ssr medical college, poste de flacq, Flacq, Mauritius; Alexa C. Gunsolley, Hartford Healthcare, Bridgeport, CT, United States; Rebecca A. Kennedy, Hartford Healthcare, Southbury, CT, United States; Naveed Hussain, Connecticut Children's Medical Center, Farmington, CT, United States
- SS
Shikha Sarkar, MBBS, DCH, MD (she/her/hers)
Associate Clinical Professor
Connecticut Children's Medical Center
West Hartford, Connecticut, United States
Presenting Author(s)
Background: An unacceptably high incidence of central-line associated bloodstream infections (CLABSI) prompted a QI initiative at the FLACQ NICU in Mauritius. QI methods were introduced by the visiting Connecticut Children’s Center for Global Health in March 2023, a local QI team was organized. Pareto analysis of baseline data determined that the greater use of central lines related to a conservative feeding regimen may be an important risk factor. A QI Program was initiated in March 2023, with the SMART
Aim: Reduce the use of central lines in admitted premature neonates by 25% within 12 mos. by the strategy of instituting standardized feeding guidelines.
Objective: 1. Determine frequency of use of central lines (umbilical arterial or venous lines or PICC lines)
2. Determine a) incidence of CLABSI & b) use of secondary antibiotics for suspected late-onset sepsis
Process measures: a) time to initiation of 1st feed after birth; b) time to reach full enteral feeds ≥ 150 ml/kg/d.
Balancing measures: a) incidence of NEC and b) incidence of aspiration pneumonia.
Design/Methods: FLACQ Hospital QI team developed a standardized feeding initiation and advancement protocol under the guidance of the CCMC team. Guidelines for central line placement and initiation of antibiotics were also standardized. Specific data-gathering forms were developed to document the variables of interest. Baseline data was obtained from the previous year (April '22–March '23). NICU staff was educated on the rationale, details of the new feeding protocol, the new guidelines for central lines & feeding strategies were implemented on April 1, 2023.
Results: Preterm neonates > 1500g birthweight (n=33):
Decrease the no. UVC insertions by 70%
Avg hrs to initiate feeds dropped from 30.2 to 9.9 hrs
Avg days to reach full feeds dropped from 8.9 to 4.9 days
Babies requiring 2nd line antibiotics dropped from 63 to 14%
No increase in NEC & aspiration pneumonia
Preterm neonates 1–1.5 kg birthweight (n=33):
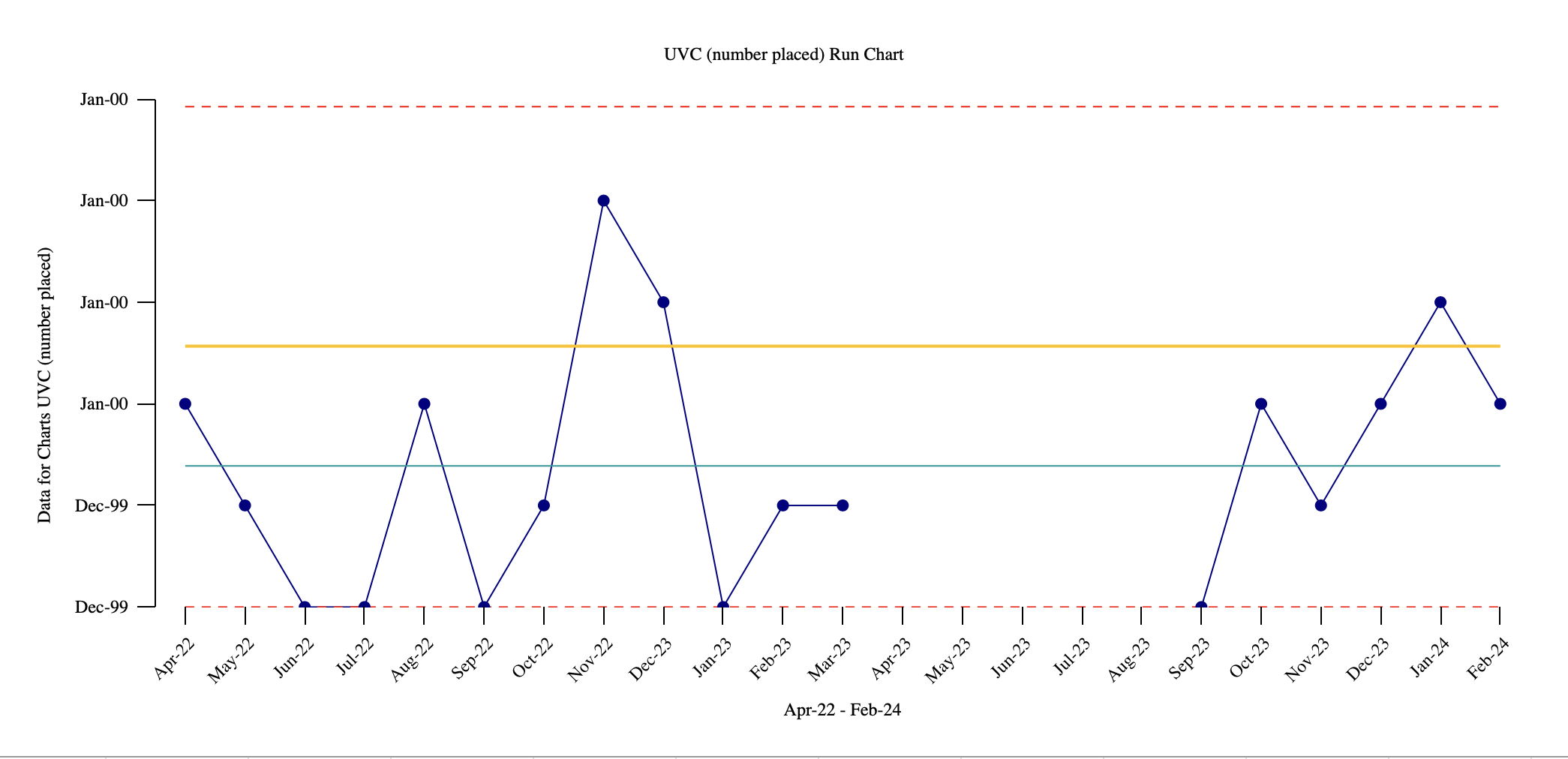
UVC insertion dropped from 100 to 80% (Fig 1)
PICC insertion dropped from 82 to 10%
Babies requiring 2nd line antibiotics dropped from 91 to 30% (Fig 2)
Hrs to initiate feeds dropped from 27.5 to 9.2 hrs (Fig 3)
Avg days to reach full feeds dropped from 11 to 5.4 days
Prefeed OGT/NGT feed aspiration dropped from 100 to 10%
No increase in the incidence NEC & aspiration pneumonia
Conclusion(s): Implementing a standardized feeding initiation & advancement protocol resulted in earlier initiation, safe advancement of feeds, decreased the need for central lines & secondary antibiotics for late sepsis & CLABSI.
Figure 2: Number of babies requiring 2nd line antibiotics Run Chart
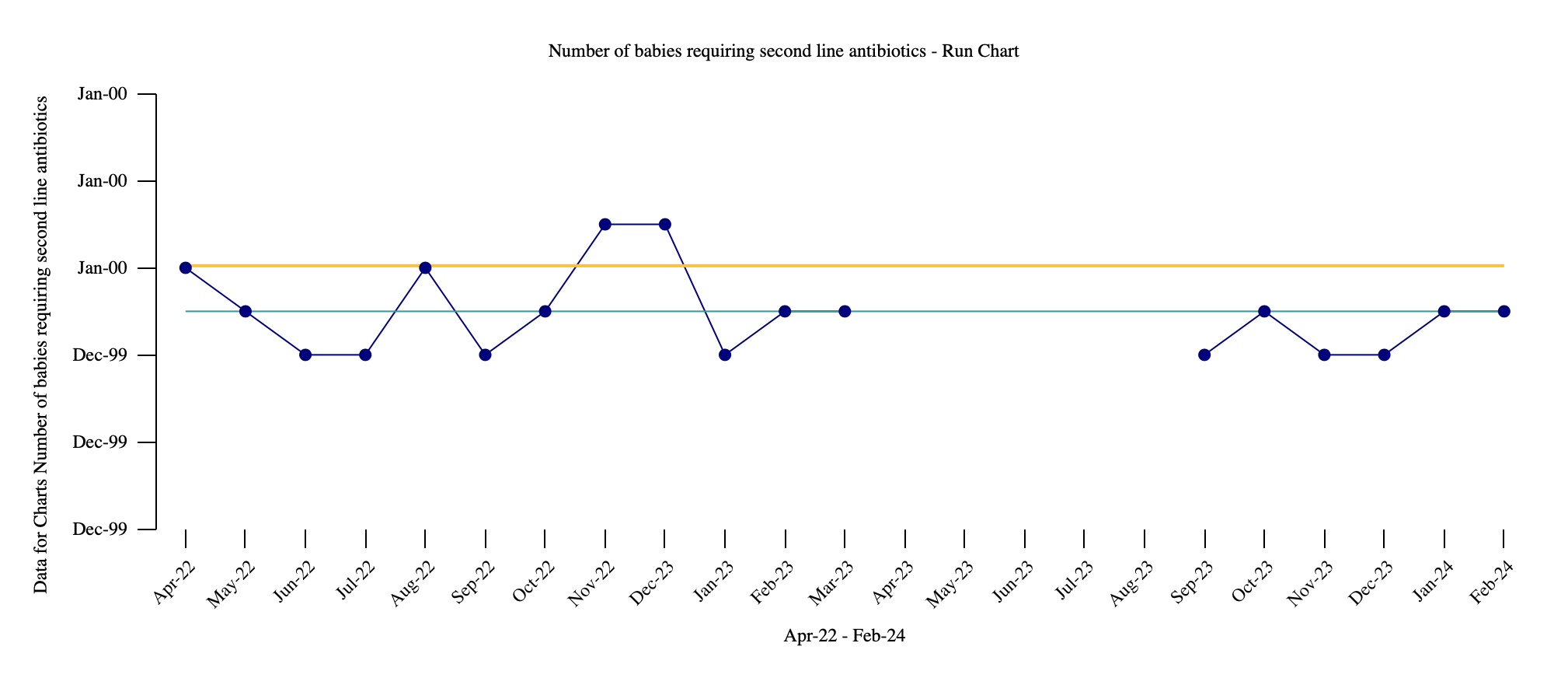
Figure 3: Average Hours Taken to Initiate Feeds Run Chart
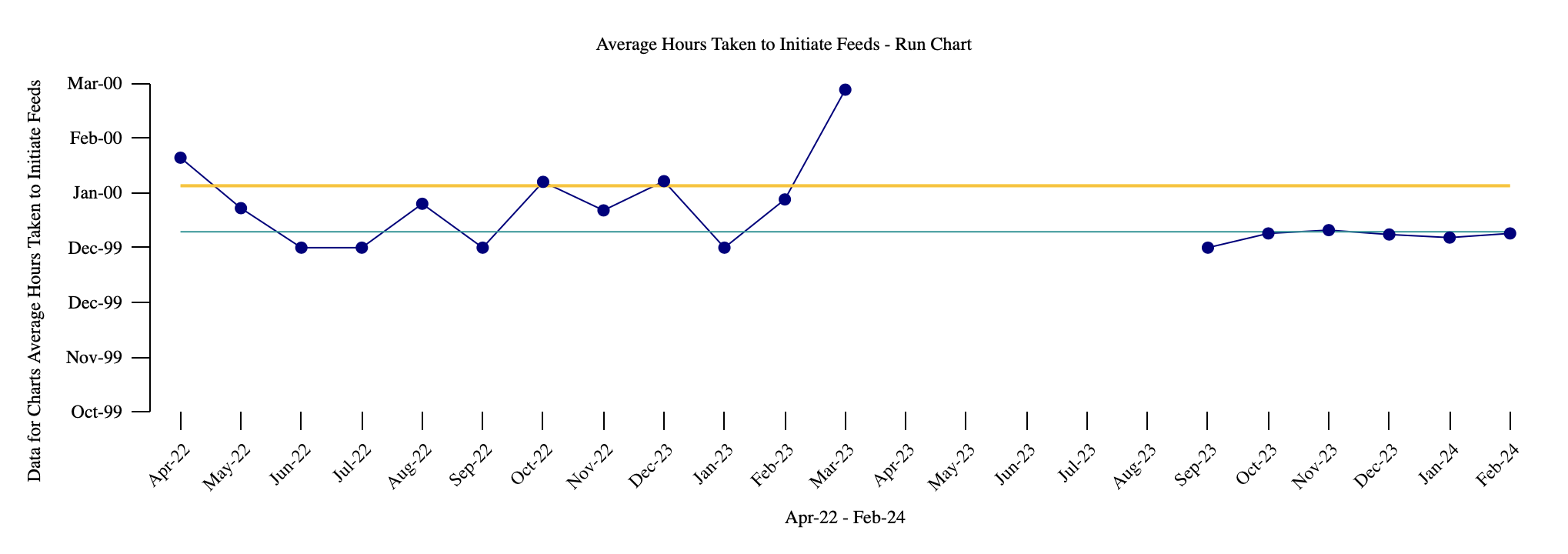
Figure 1: UVC Placement Run Chart