Hospital Medicine 6: Clinical
Session: Hospital Medicine 6: Clinical
536 - Adherence to the 2011 IDSA/AAP Pneumonia Guidelines in a Pediatric Emergency Department
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 536.3917
Akash S. Daswaney, Charleston Area Medical Center, Charleston, WV, United States; Neil Copeland, West Virginia University School of Medicine/CAMC Women and Children's Hospital, Charleston, WV, United States; Stephanie Thompson, Charleston Area Medical Center, Charleston, WV, United States

Akash S. Daswaney (he/him/his)
Resident Physician, PGY-III
Charleston Area Medical Center
Charleston, West Virginia, United States
Presenting Author(s)
Background: Pneumonia is a leading cause of pediatric illness globally, impacting 1.45 per 1,000 children under 16 annually. The American Academy of Pediatrics (AAP) and Infectious Disease Society of America (IDSA) published joint guidelines in 2011 for managing community-acquired pneumonia (CAP) in children older than 3 months. The AAP Section on Emergency Medicine Committee on Quality Transformation (ASEMCQT) further refined these guidelines, offering a treatment algorithm based on disease severity. Our study includes the COVID-19 pandemic period to assess its influence on CAP management practices.
Objective: To assess adherence to the IDSA/AAP guidelines for managing community-acquired pneumonia in children within the pediatric emergency department (ED).
Design/Methods: We conducted a retrospective chart review of pediatric patients (ages 3 months to 18 years) diagnosed with CAP in our institution's ED from 2017 to 2021. Exclusion criteria included CAP not being the primary diagnosis, underlying pulmonary disease, home mechanical ventilation, immunocompromise, or complicated disease presentation. Adherence was evaluated based on diagnostic workup, antibiotic selection, and patient disposition—statistical analyses, including Chi-squared and Fisher exact tests, assessed group differences.
Results: Out of 300 children (25 excluded), 78% had mild presentations, and 22% were moderate/severe, with a median age of 3 years.
Antibiotic prescription occurred in 92% of cases, aligning with guideline-recommended agents (amoxicillin, azithromycin, ceftriaxone) only 31% of the time (37% in mild vs. 0.1% in moderate/severe cases).
Chest X-rays were used appropriately in 50% of cases, though overutilized in 63% of mild cases.
No significant difference was observed in guideline adherence or investigation frequency based on insurance type or follow-up capability. Post-COVID, NP swab usage increased (73% vs 55%).
Conclusion(s): While patient disposition often adhered to ASEMCQT recommendations, diagnostic workups, and antibiotic selection reflected areas for improvement. Findings highlight the need for system-based strategies emphasizing antimicrobial stewardship, radiation minimization, and consistency in CAP management across pediatric emergency settings.
Adherence to AAP Guidelines for Diagnostic Testing in Pediatric CAP Cases, Stratified by Disease Severity
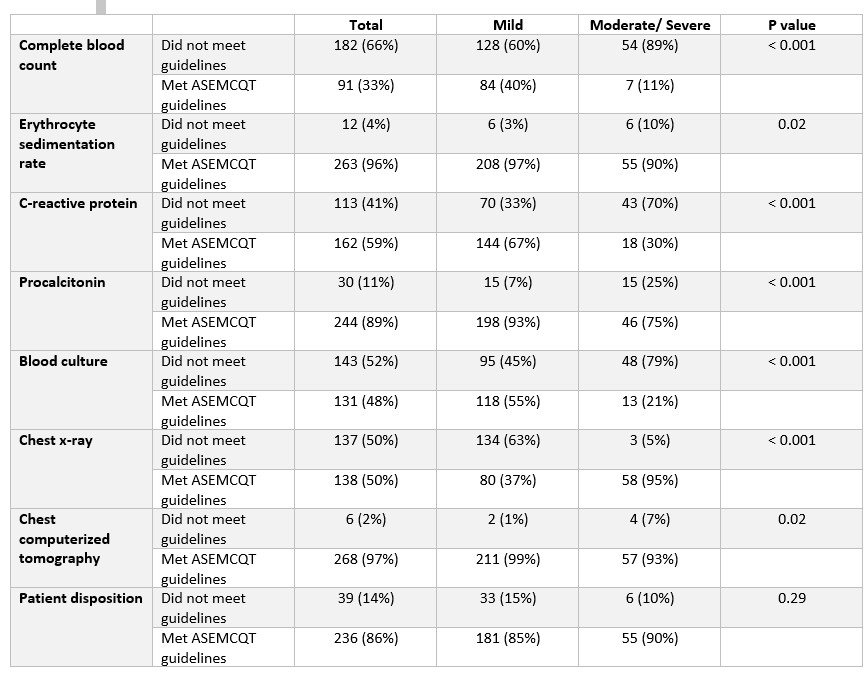 Complete blood count (CBC) and blood culture were ordered in disagreement with guidelines 66% and 52% of the time.
Complete blood count (CBC) and blood culture were ordered in disagreement with guidelines 66% and 52% of the time. Inflammatory markers showed mixed adherence.
Chest X-rays were overutilized in mild cases (63%), while patient disposition adhered to guidelines 86% of the time.
Compliance with AAP Guidelines for Antibiotic Use in Pediatric CAP Cases, Stratified by Disease Severity
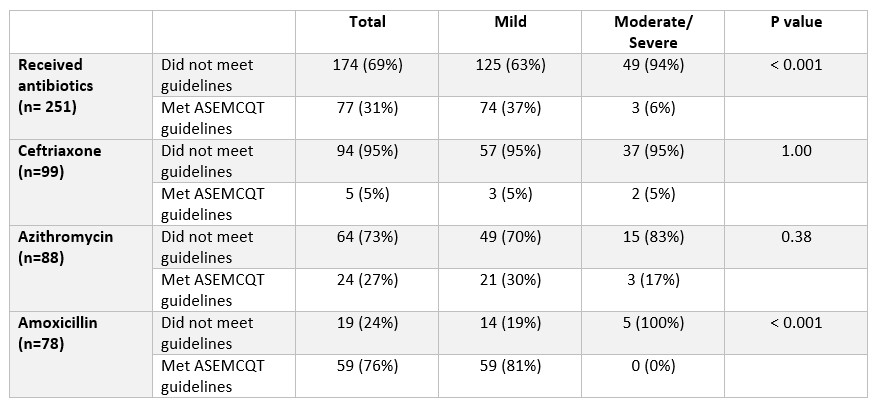 Overall, antibiotics were prescribed in disagreement with the guidelines 69% of the time, with higher non-adherence in moderate/severe cases (94%) compared to mild (63%).
Overall, antibiotics were prescribed in disagreement with the guidelines 69% of the time, with higher non-adherence in moderate/severe cases (94%) compared to mild (63%). However, narrow-spectrum antibiotic utilization (amoxicillin) occurred per the guidelines 76% of the time.

