Global Neonatal & Children's Health 6
Session: Global Neonatal & Children's Health 6
809 - Validating and Piloting a Pediatric Respiratory Distress Knowledge Survey: A Systematic and Cross-Cultural Approach
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 809.7078
Sophia Figueroa Katz, Stanford University School of Medicine, Palo Alto, CA, United States; Iliana R. Close, Stanford University School of Medicine, San Carlos, CA, United States; Kelly Tellez, Stanford University School of Medicine, Palo Alto, CA, United States; Monique de Araujo, Stanford University School of Medicine, Mountain View, CA, United States; Alejandra Ximena Rojas Garcia, UNAM, organization: Parteria y Medicinas Ancestrales, Refugee Health Alliance non profit., Chula vista, CA, United States; Maggi Smeal, Gardner Packard Children's Health, palo alto, CA, United States; Psyche Calderon, Universidad Autónoma de Baja California, Tijuana, Baja California, Mexico; Ben Domingue, Stanford University, Stanford, CA, United States; Rishi Mediratta, Stanford University School of Medicine, Palo Alto, CA, United States
- SF
Sophia Figueroa Katz, MD (she/her/hers)
Resident Physician
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background: Pediatric respiratory distress (PRD) is a leading cause of child mortality in resource-limited settings. Early recognition and appropriate management are crucial for improving outcomes. However, health workers in these settings often lack the training to identify PRD.
Objective: To develop and validate a survey to assess knowledge of PRD and to pilot an instructional video curriculum to improve knowledge among health workers in resource-limited settings.
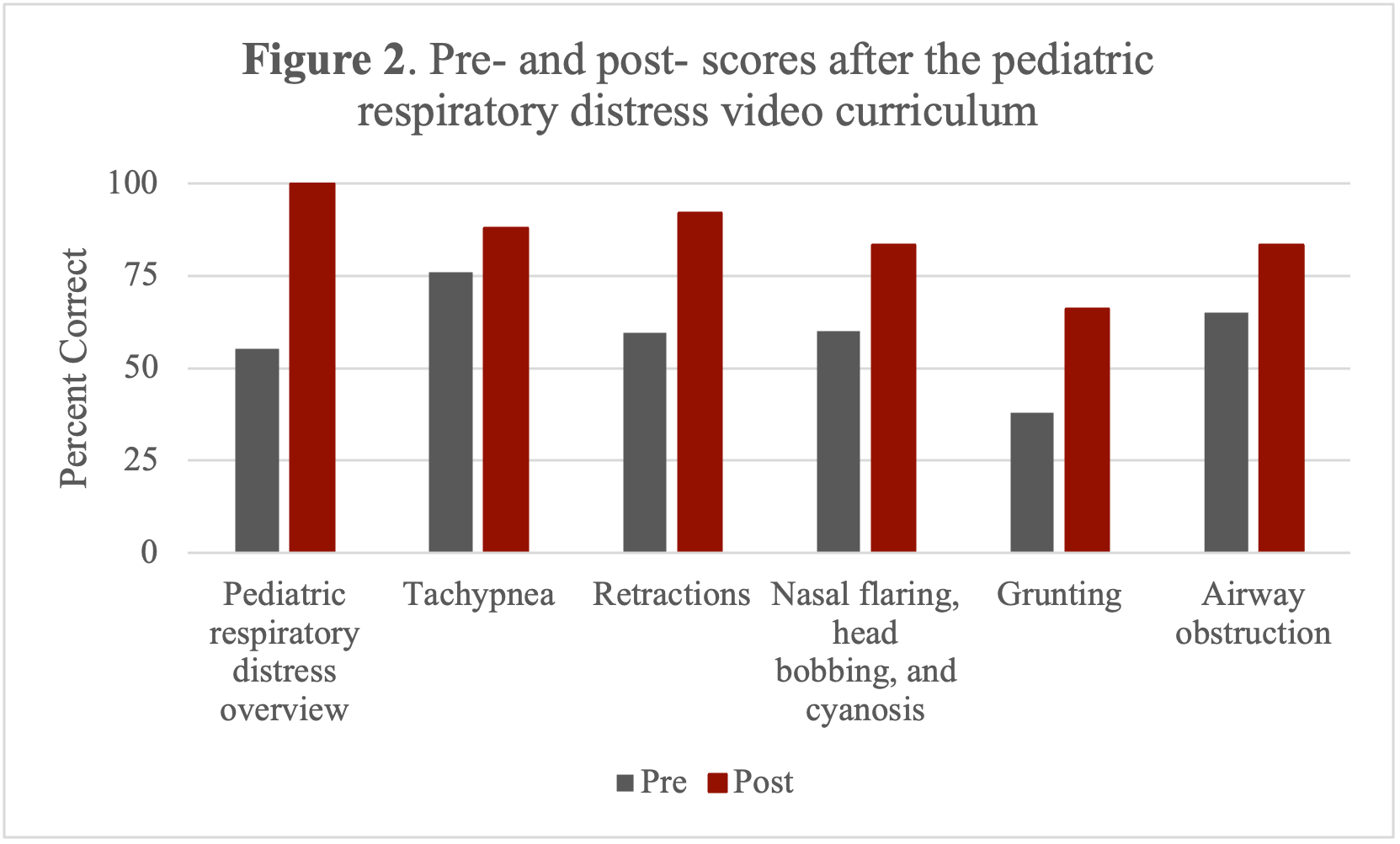
Design/Methods: We previously created a video curriculum for health workers to recognize PRD. We developed an IRB-exempt survey to assess knowledge gained from the curriculum using Artino’s seven-step approach (Figure 1), incorporating a literature review and input from Ethiopian providers. Experts in pediatrics, emergency medicine, critical care, and respiratory therapy from the U.S., Ethiopia, India, Tanzania, Rwanda, and Mexico reviewed the survey for content, relevance, and clarity. Response process validity was evaluated through cognitive interviews with pediatricians from Tanzania, Ethiopia, Colombia, and Honduras. The survey was translated to Spanish and piloted with health workers (n=10) at Refugee Health Alliance clinics in Mexico. Pre- and post-curriculum knowledge about PRD was analyzed using the Wilcoxon signed-rank test.
Results: After 21 experts reviewed the survey and eight cognitive interviews were conducted, we selected 31 questions divided into six modules: 1) PRD overview, 2) tachypnea, 3) retractions, 4) nasal flaring, head bobbing, and cyanosis, 5) grunting, and 6) airway obstruction. Based on the cognitive interviews, we simplified the language and clarified answer choices, improving the survey’s usability across diverse linguistic backgrounds. All pilot study participants (n=10, Table 1) demonstrated improved survey total scores after completing the curriculum. The proportion of total correct responses increased from 67% (95% CI 59%-75%) pre-intervention to 85% (95% CI 78%-92%) post-intervention (p=0.005). Scores improved across all six modules (Figure 2).
Conclusion(s): This structured approach generated validity evidence for a survey assessing knowledge of PRD. Our pilot suggests that our video curriculum improved knowledge about PRD recognition among health workers in a resource-limited setting. The curriculum benefited individuals with diverse professional backgrounds and levels of experience. Larger studies are needed to further validate the effectiveness of the curriculum and its generalizability in different global settings.
Figure 1. Artino’s 7-Step Validation Process
.png)
Table 1. Socio-demographic characteristics of Refugee Health Alliance pilot participants (n=10).
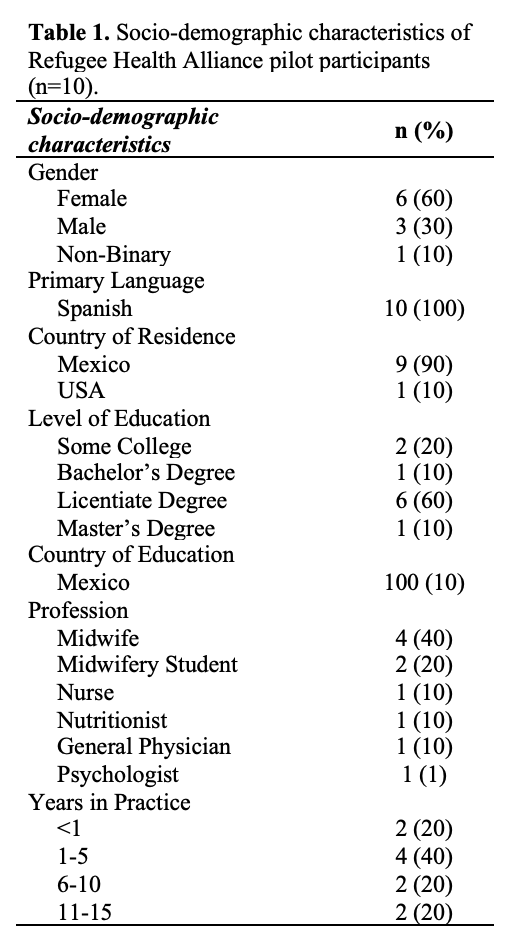
Figure 2. Pre- and post- scores after the pediatric respiratory distress video curriculum