Children with Chronic Conditions 1
Session: Children with Chronic Conditions 1
503 - Validity of Caregiver-Collected Tracheostomy Aspirate Culture Testing in Children with Tracheostomies
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 503.7085
Rebecca Steuart, Medical College of Wisconsin, Milwaukee, WI, United States; Blake W. Buchan, Medical College of Wisconsin, Milwaukee, WI, United States; Elaina Schueler, Medical College of Wisconsin, Milwaukee, WI, United States; Jennifer Henningfeld, Medical College of Wisconsin, Milwaukee, WI, United States; Kelly M. Day, Children's Wisconsin, Wauwatosa, WI, United States; Kaitlin A. Kunz, Childrens Wisconsin, Milwaukee, WI, United States; Amy Pan, Medical College of Wisconsin, Milwaukee, WI, United States; Liyun Zhang, Medical College of Wisconsin, Wauwatosa, WI, United States; Cecilia Lang, Children's Hospital of Wisconsin, Milwaukee, WI, United States; Michelle Mitchell, Medical College of Wisconsin, Milwaukee, WI, United States; Joanne Lagatta, Medical College of Wisconsin, Milwaukee, WI, United States; David Brousseau, Nemours Children's Hospital, Wilmington, DE, United States

Rebecca L. Steuart, MD, MS (she/her/hers)
Assistant Professor of Pediatrics
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Sporadic surveillance respiratory culture testing of tracheostomy aspirates (TA) likely overlooks shifts in bacterial communities and makes diagnosing airway colonization challenging. Frequency of culture surveillance is limited by the need for a medical professional to collect the sample.
Objective: To evaluate the acceptability and concordance of TA respiratory cultures from samples collected by caregivers vs. clinic staff on the same day.
Design/Methods: This prospective study included children 2 months-18 years old with tracheostomies and their caregivers attending routine pulmonary clinic visits. Children in foster care and those with non-English speaking caregivers were excluded. Caregivers received in-person, video, and written education for sterile TA culture collection (goal ≥1mL mucus) with a mucolytic transport medium. Caregiver-collected and staff-collected TA cultures were obtained on the day of subsequent routine clinic visits. Caregivers were surveyed pre- and post-collection for comfort, acceptability, and confidence in sample quality. Paired samples underwent Gram stain, bacterial culture, and organism identification per routine protocols by technologists blinded to collector. Paired culture results were compared for qualitative species concordance using positive and negative percent agreement (PPA, NPA) and the degree of agreement was measured by Cohen’s kappa(k).
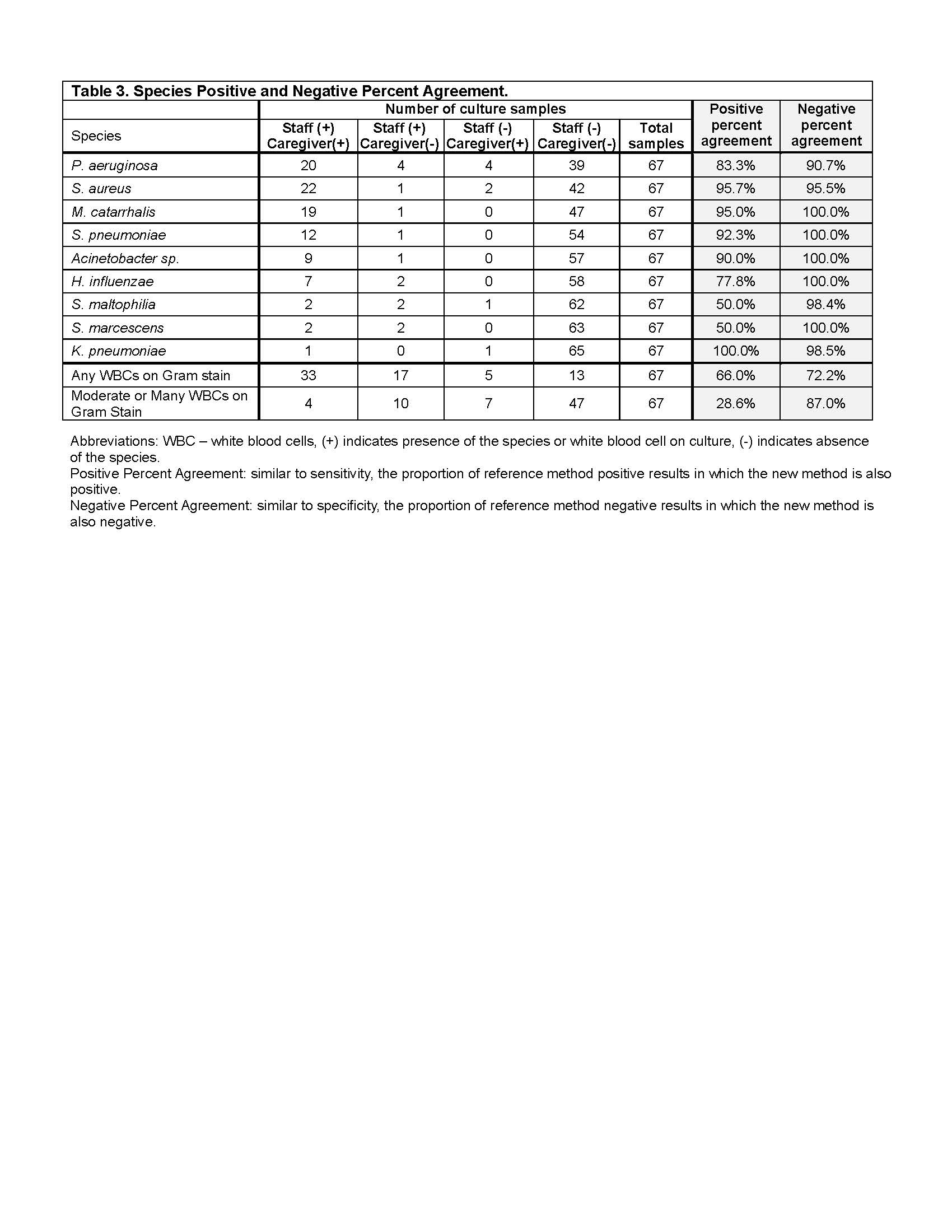
Results: We collected 68 TA caregiver/staff sample pairs from 39 children (median 2 pairs per child, range 1-4, Table 1). Children were a median 3.6 years old (IQR 2.2-9.1) and 31% used chronic ventilation. Caregivers were mostly female (82%) parents (92%) without a college degree (48%). Most reported collection was comfortable/very comfortable (85%) and acceptable/very acceptable (82%, Table 2). 1 sample was discarded due to sampling error. Overall, 82% of staff- and 87% of caregiver-collected cultures had ≥1 organism. Staff-collected cultures identified 151 isolates; caregiver-collected cultures identified 144. We identified qualitative concordance rates of 97%, 90%, and 85% for the 1st, 2nd, and 3rd most abundant species cultured in each pair (k=0.95, 0.87, 0.63 respectively). Most species had fair to excellent PPA between sample pairs, and all had excellent NPA (Table 3).
Conclusion(s): Caregiver collection of TA samples yields substantially equivalent culture results to staff-collected samples and appears to be acceptable to caregivers. Empowering caregivers to collect samples at home will allow for a more comprehensive understanding of respiratory colonization and advance respiratory infection diagnosis and treatment.
Table 1. Caregiver Population.
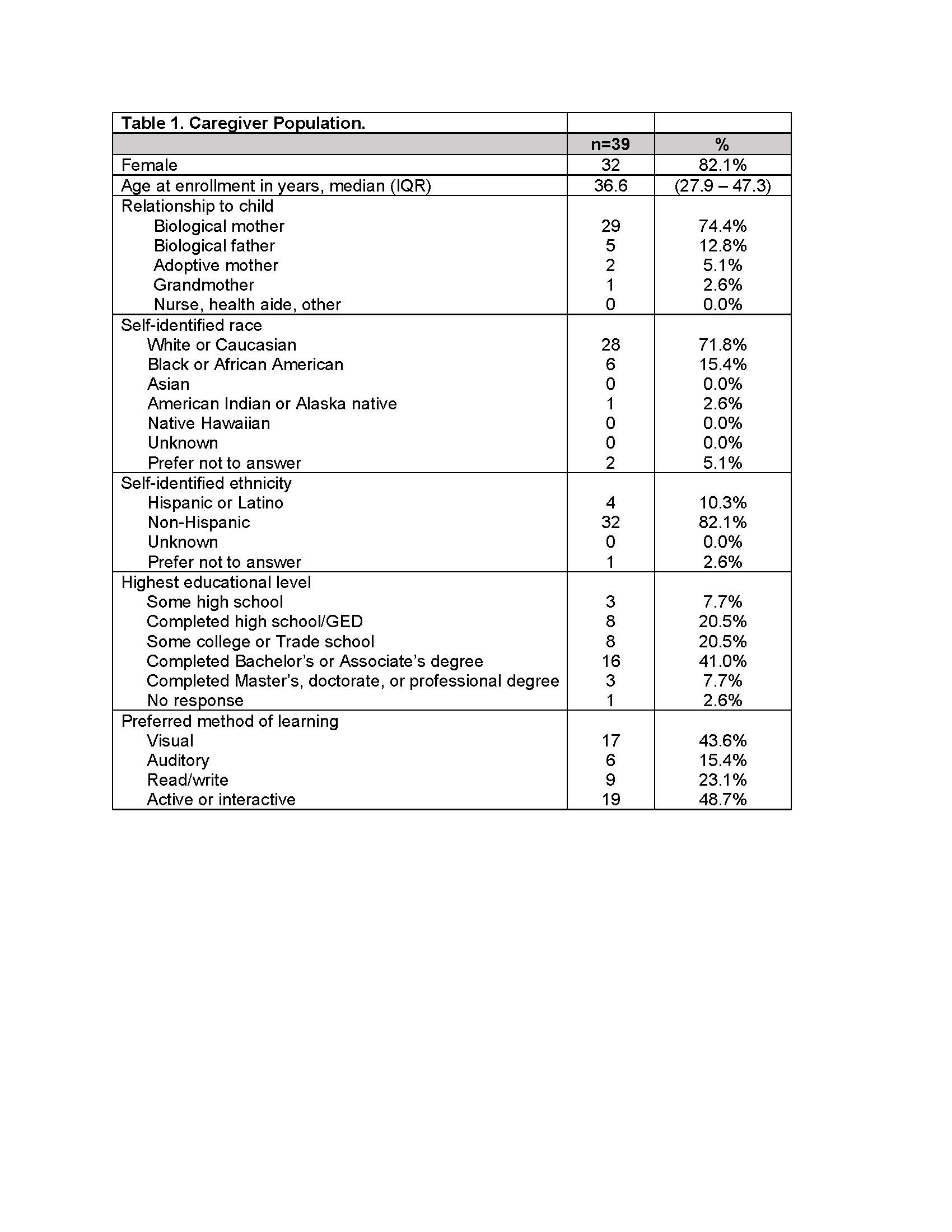
Table 2. Caregiver-Collected Culture Details and Caregiver Opinion Surveys.
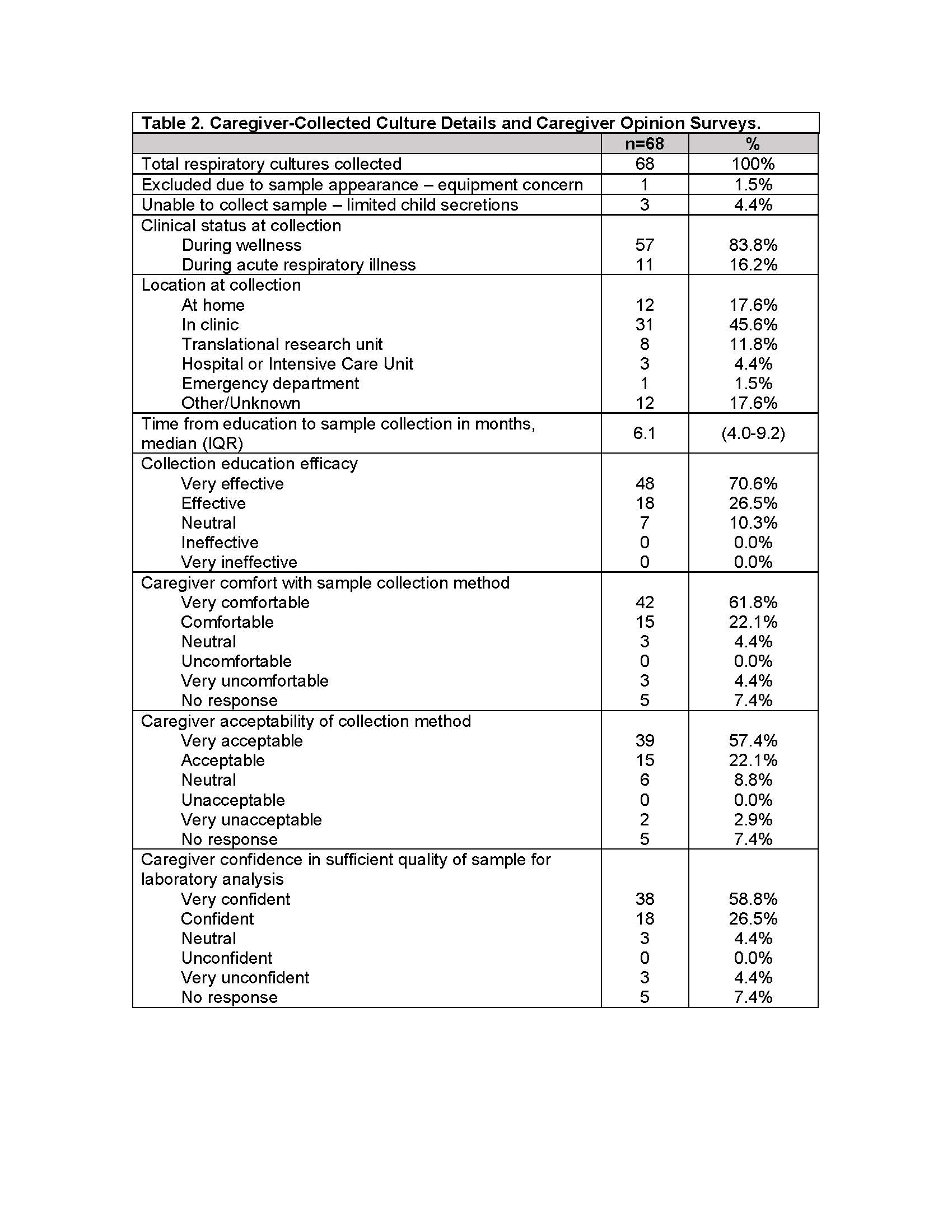
Table 3. Species Positive and Negative Percent Agreement.