Hospital Medicine 5: Clinical
Session: Hospital Medicine 5: Clinical
533 - Variation in Admission and Treatment Decisions for Previously Immunocompetent Pediatric Patients Presenting to the ED with Febrile Neutropenia
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 533.7048
Brianna Leyden, CHOC Children's Hospital of Orange County, Santa Ana, CA, United States; Ricardo Aguilar, CHOC Children's Hospital of Orange County, Orange, CA, United States; Britanny Winckler, University of California, Irvine, School of Medicine, Orange, CA, United States; Jennifer Lusk, CHOC Children's Hospital of Orange County, Orange, CA, United States

Brianna Leyden, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
CHOC Children's Hospital of Orange County
Santa Ana, California, United States
Presenting Author(s)
Background: Patient volumes limit studies of immunocompetent pediatric patients with febrile neutropenia; no guideline consensus exists. Extrapolating serious bacterial infection (SBI) risk from other populations leads to resource overutilization.
Objective: We quantified practice variation in emergency department (ED) disposition for immunocompetent pediatric patients with febrile neutropenia. We evaluated which factors increase admission odds and the association of disposition and SBIs.
Design/Methods: We performed a retrospective study using the de-identified multicenter database Cerner Real-World Data. ED patients ages 2 months – < 18 years from January 2016-June 2023 with an absolute neutrophil count (ANC) < 1500 and temperature > 38° C were included. Encounters resulting in transfer or death or with diagnoses of neoplasms, immunocompromised status, or implanted devices were excluded. A logistic regression mixed effects model determined the variance partition coefficient (VPC), the proportion of variance explained by health systems differences, and what factors increase admission odds. Univariate analysis (chi-squared and Fisher’s exact tests) examined the association of ED disposition and rates of sepsis/SIRS or SBIs (bacteremia, bacterial meningitis, or urinary tract infection) within 5 days of presentation.
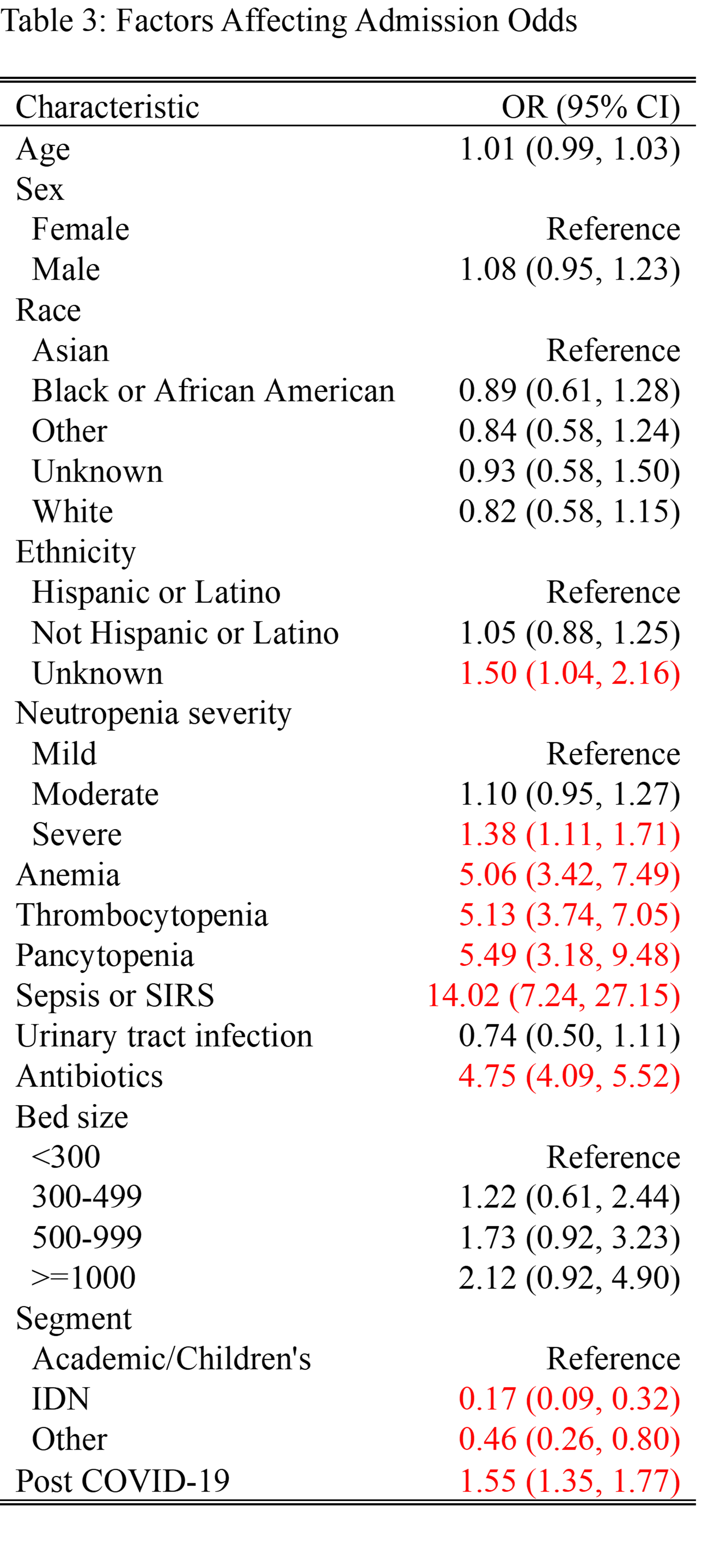
Results: Of 5,544 qualifying ED encounters — 60.6% at an Academic/Children’s center, 28.2% Integrated Delivery Network (IDN), 11.1% other — 41.9% resulted in admission. Median patient age was 1.43 years, with 53.8% male and 60.1% White. Neutropenia was classified as 57.2% mild, 30.3% moderate, and 12.5% severe. Estimated VPC is 8% (Table 1). Diagnoses of sepsis/SIRS (p < 0.001), bacteremia (p < 0.001), and bacterial meningitis (p = 0.002) were more likely in admitted encounters (Table 2). Only bacteremia was associated with discharged encounters. Multiple factors increased admission odds: diagnoses of sepsis/SIRS (OR 14.02), pancytopenia (5.49), thrombocytopenia (5.13), and anemia (5.06); if antibiotics were given (4.75); and system characteristics of children’s hospital encounter (IDN 0.17 and other 0.46 versus Academic/Children’s) and after the COVID-19 pandemic (1.55) (Table 3).
Conclusion(s): Our study showed that variation in practice is relatively low. Patients with SBIs are more likely to be admitted, suggesting providers correctly identify at-risk patients. Further studies should elucidate the association between ED discharge and bacteremia. With validation of factors associated with increased admission, a safe clinical practice guideline to optimize outcomes and decrease overutilization is possible.
Proportion of Admission Variance by Health Systems Differences
.png)
Table 2: Association between Admission Status and Diagnosis Code
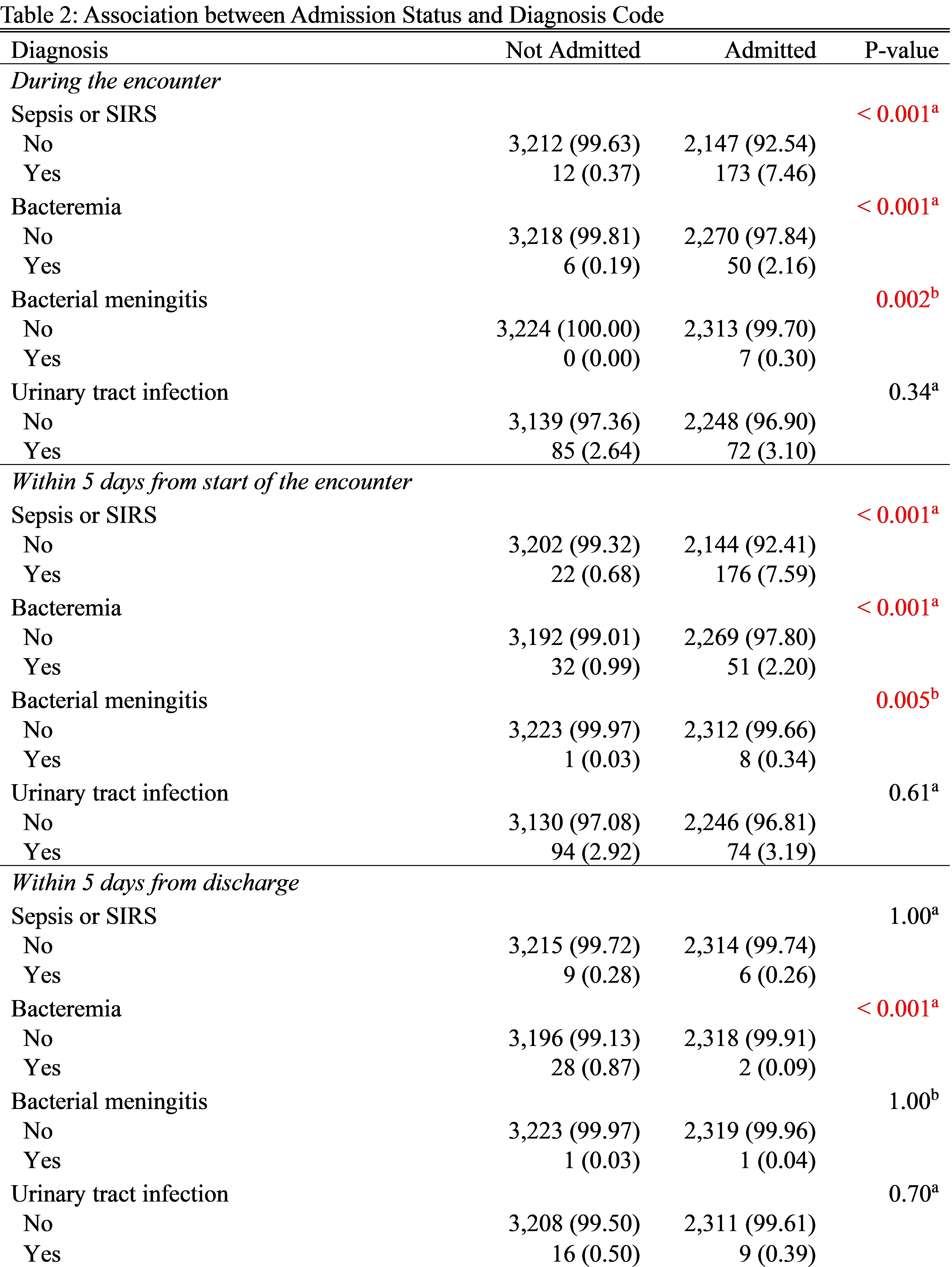
Table 3: Factors Affecting Admission Odds