Health Equity/Social Determinants of Health 6
Session: Health Equity/Social Determinants of Health 6
736 - The Role of Socioeconomic Status in Pediatric Respiratory Outcomes During Wildfire Exposure
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 736.6790
Allison Henning, Stanford University School of Medicine, Palo Alto, CA, United States; Andy Y. Wen, Lucile Packard Children's Hospital Stanford, Palo Alto, CA, United States; Daniel Tawfik, Stanford University School of Medicine, Palo Alto, CA, United States; Anna Lin, Stanford School of Medicine, Stanford, CA, United States; John W. Grunyk, Stanford Children’s Hospital, Palo Alto, CA, United States; Melanie Stroud, Lucile Packard Children's Hospital Stanford, Palo Alto, CA, United States

Allison Henning, DO (she/her/hers)
Pediatric Critical Care Fellow
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background: Wildfires pose an escalating global threat, exposing over 2 billion people annually to hazardous air quality. During wildfires, children from low socioeconomic status (SES) regions often experience worse respiratory outcomes than their higher SES peers. However, data linking these outcomes directly to wildfires remains limited.
Objective: This study investigates whether wildfires exacerbate disparities in respiratory health outcomes when compared to non-wildfire periods.
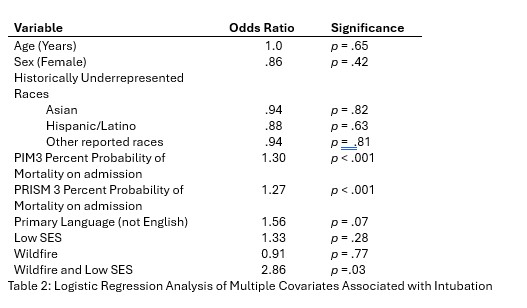
Design/Methods: This retrospective cohort study analyzed data from 2,417 patients aged 0-29 years who were admitted to a quaternary Pediatric Intensive Care Unit (PICU) for acute respiratory failure between 2016 and 2023. Data were sourced from Virtual Pediatric Systems, the Area Deprivation Index (ADI), Fire Information for Resource Management, and Air Quality System, using zip codes for merging.
The Wildfire cohort included children with (1) the presence of a wildfire within 100 miles, confirmed by satellite images, and (2) PM2.5 levels in the 10 days prior to admission at least 1 standard deviation above the annual mean. The non-Wildfire cohort consisted of all other children admitted during the same period.
SES was categorized using ADI with low and high SES defined as the lowest and highest quintiles, respectively. Fisher’s exact test, Mann-Whitney U test, and logistic regression analyses were used to compare outcomes between groups.
Results: During wildfires, children from low SES backgrounds faced a significantly higher absolute risk of intubation compared to non-wildfire periods (29% vs. 13%, p = .003). This was not observed among children from high SES backgrounds (8% vs 10%, p = 0.49). Logistic regression analysis revealed that the interaction between wildfire exposure and low SES substantially increased the odds of intubation (OR = 2.7, p = .04)
Severity of illness, as measured by higher Pediatric Index of Mortality 3 (PIM3), was associated with increased odds of intubation (OR = 1.3, p < .001). Notably, other demographic factors including age, sex, race, and primary language did not show statistically significant associations with intubation risk.
Conclusion(s): This study highlights disparities in outcomes for children from low SES backgrounds during wildfires, with low SES linked to more severe respiratory outcomes from wildfire-related pollution. Additional research and greater public health awareness can inform targeted interventions and disaster preparedness to protect these vulnerable populations.
Table 1: High and Low Socioeconomic status cohorts for Wildfire vs Non-Wildfire Times
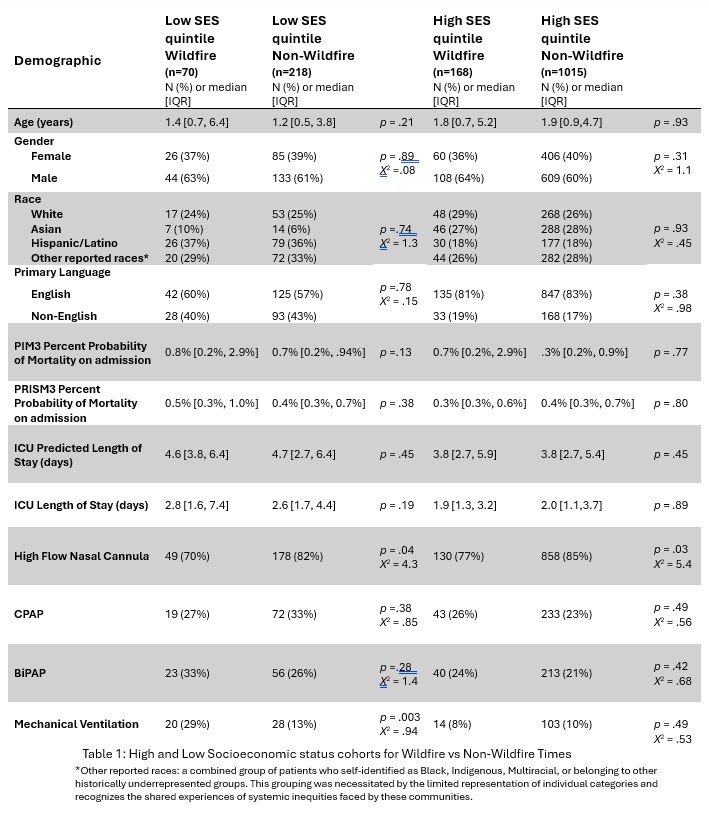
Table 2: Logistic Regression Analysis of Multiple Covariates Associated with Intubation