Sedation Medicine
Session: Sedation Medicine
583 - The Perfect Match – A Patient-Centered Approach to Pediatric Sedation
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 583.6765
SAMRAT U. DAS, Duke University School of Medicine, DURHAM, NC, United States; Emily Sterrett, Duke University School of Medicine, Durham, NC, United States
Samrat U. Das, MD (he/him/his)
Professor of Pediatrics
Duke University School of Medicine
DURHAM, North Carolina, United States
Presenting Author(s)
Background: Children often require a broad range of behavior supports in order to cooperate with diagnostic testing. To meet some of these needs, the Children’s Procedural Sedation Unit at our institution provided moderate sedation services for elective outpatient imaging. To expand services to meet the needs of more children, the CPSU initiated a project in July 2022 to safely improve the efficiency of diagnostic testing for all children.
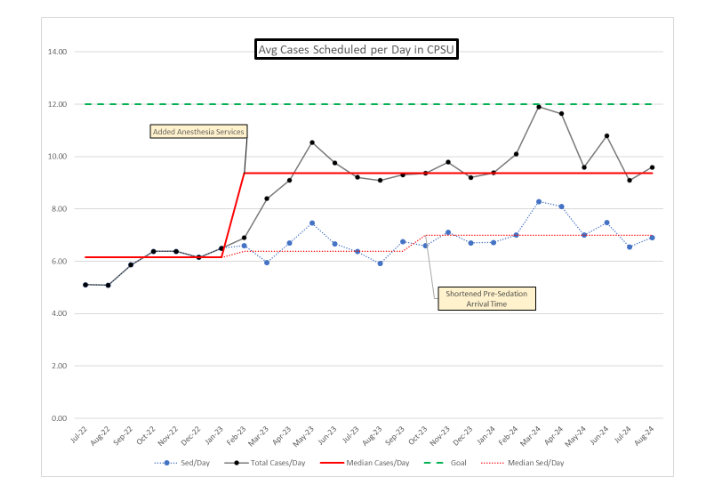
Objective: The primary aim was to increase the average number of pediatric sedation cases scheduled in the CPSU from 5 to 12 patients per day by December 2024 while maintaining a commitment to patient-centered approaches.
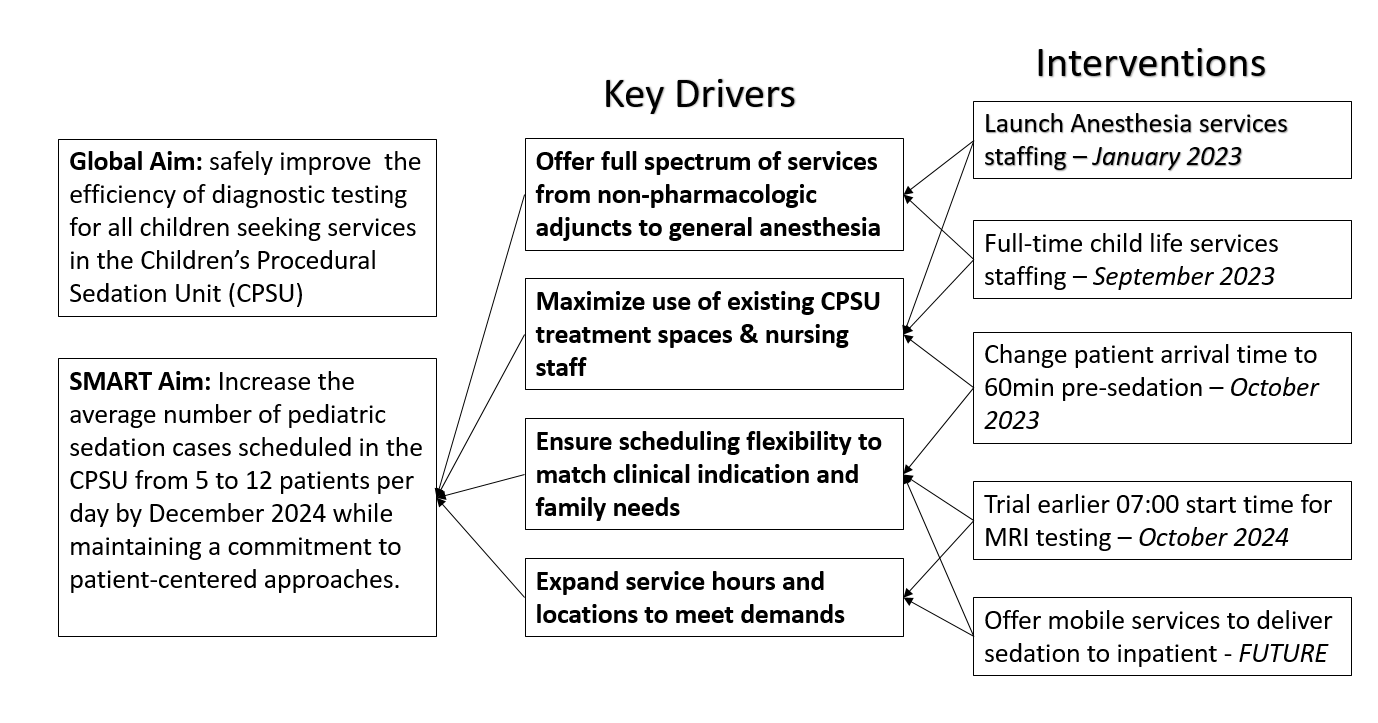
Design/Methods: A multidisciplinary team convened to identify opportunities and strategies to enhance efficiency using Model for Improvement methodology (Key Driver Diagram). Stakeholders included child life services, emergency medicine, hospital medicine, anesthesiology, nursing, radiology and hospital administration. Key interventions included launching pediatric general anesthesia services, employing a full-time Child Life Specialist, and reducing pre-sedation arrival times from 90 to 60 minutes. Outcome and balancing measures were tracked monthly, including the average number of patients scheduled each day, the monthly number of children not requiring medication (child life services only), and the no-show or cancellation rate.
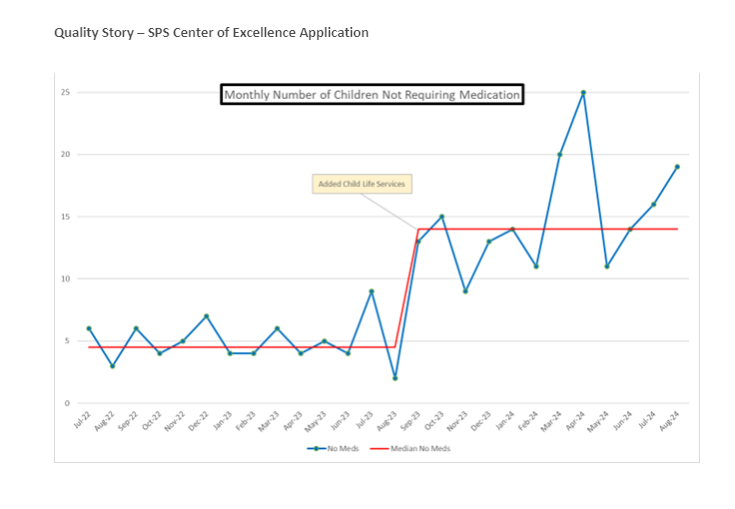
Results: Following the launch of pediatric general anesthesia services, the average daily scheduled pediatric sedation cases increased from 6.1 to 9.4 patients. The involvement of the Child Life Specialist significantly improved support for patients undergoing sedation, leading to an increase in those completing procedures without medication, rising from 4.5 to 14 per month. Additionally, the reduction in pre-sedation arrival times boosted the number of daily scheduled pediatric sedations from 6.4 to 7, with a stable no-show rate of 1.5 patients per day.
Conclusion(s): This initiative effectively improved access to the CPSU for diagnostic testing for pediatric patients requiring behavioral supports ranging from child life services to moderate sedation to general anesthesia. These efforts represent generalizable opportunities to enhance both capacity and patient-centered care by aligning pediatric sedation practices with the unique needs of all children and their families.
Key Driver Diagram
Average Cases Scheduled per day in CPSU
Monthly number of Children Not Requiring Medication