Children with Chronic Conditions 1
Session: Children with Chronic Conditions 1
499 - Self-management in the Context of Psychosocial Health: A Qualitative Descriptive Study of Adolescents with Chronic Conditions
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 499.6224
Katherine Melton, Boston Children's Hospital, Boston, MA, United States; Kira K. Fried, Boston Children's Hospital, North Yarmouth, ME, United States; Mimi Stotsky, Boston Children's Hospital/Harvard Medical School, Boston, MA, United States; Jean Connor, Boston Children's Hospital, Boston, MA, United States; Gregory S.. Sawicki, Harvard Medical School, Boston, MA, United States

Katherine Melton, PhD, BSN (she/her/hers)
Research Fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Adolescents with chronic conditions are at risk for poor health outcomes related to unsuccessful self-management. However, the influence of peers and other psychosocial factors on self-management is poorly understood.
Objective: To describe the interaction between psychosocial factors and self-management behaviors among adolescents living with chronic health conditions to identify targets for intervention.
Design/Methods: Guided by qualitative descriptive methodology, we purposively sampled adolescents (12-17 years) with ≥1 chronic health condition from a single children’s hospital. We conducted semi-structured video or phone interviews which were transcribed and independently coded by 2 researchers. An iterative codebook guided conventional content analysis and coders meet weekly to resolve discrepancies.
Results: 24 adolescents with a range of chronic conditions participated (see Table 1). The overarching theme: Self-management in the Context of Psychosocial Health was characterized by six subthemes. 1) Multidimensional Support Needs: Comprehensive support from peers, family, and school is needed to support psychosocial health and self-management behaviors. 2) Excluded, Targeted, and Misunderstood: Across conditions adolescents reported negative peer interactions and health-related bullying which affected how they viewed their diagnosis and treatments. 3) Fitting in Versus Standing Out: Participants expressed a desire to fit in and feel “normal”; changes in appearance due to condition or treatments negatively impacted body image and peer interactions. 4) To Share or not to Share: Participants often restricted how much peers knew about their health. This provided control over their illness but also limited the number of people available to provide support. 5) Taking Care of Myself: Participants expressed generally high levels of confidence in their self-management abilities; a supportive best friend often served as a key self-management facilitator by providing treatment reminders or emotional support. 6) “They know what you’re going through”: For those who had the opportunity, peer support from other chronically ill teens had a positive impact on coping and psychosocial health. Most participants were open to peer support both to discuss illness management and for general social support.
Conclusion(s): Across chronic conditions peer interactions were complex; negative peer interactions contributed to poor psychosocial health outcomes (i.e., isolation) while positive interactions served as protective factors for self-management. Targets to improve self-management were identified, specifically peer support.
Table 1: Participant Demographics
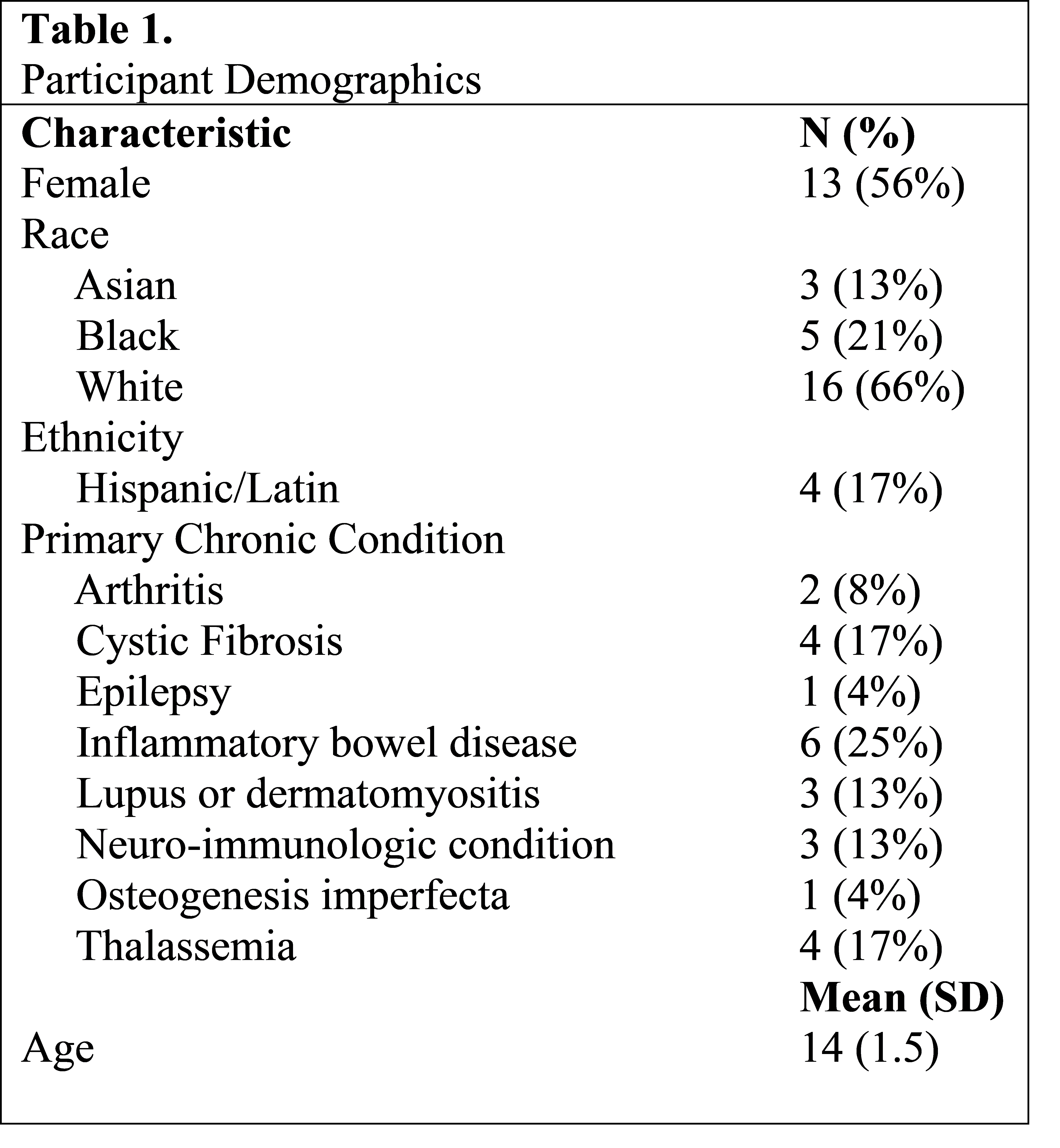
Table 2: Subthemes and Exemplar Quotes
.png)

