Emergency Medicine 8
Session: Emergency Medicine 8
120 - Pulse Oximetry as a Predictor of Outcomes in Pediatric Acute Respiratory Illness in the Emergency Department
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 120.6160
Max Ledersnaider, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Oak Park, IL, United States; Todd A. Florin, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Elizabeth Alpern, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States

Max Ledersnaider, MD (he/him/his)
Resident
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Oxygen (O2) saturation is frequently used to guide clinical decision-making for children with acute respiratory illness. There is no consensus and limited evidence in the literature on appropriate O2 saturation thresholds in pediatrics pertaining to intervention, hospitalization, or risk of deterioration.
Objective: To describe the relationship between O2 saturation and rates of return visits among children discharged from the ED with a respiratory illness.
Design/Methods: We performed a retrospective cohort study of children ( < 18 years) discharged from the ED of a quaternary care children’s hospital between 2016-2022 with an ICD-10 diagnosis code indicating respiratory illness. We excluded children with congenital cyanotic heart disease and with chronic respiratory failure. Our exposure of interest was lowest O2 saturation during the ED encounter. Outcomes included (1) any ED return visit within 7 days of the index encounter, and (2) return ED visit within 7 days leading to admission. We explored the association between O2 saturation and outcomes using a tail-restricted cubic spline function. We reported measures of diagnostic accuracy of varying cutpoints of O2 saturation with each study outcome.
Results: We included 10,832 children with a respiratory illness (58.4% male, median age 2.3 years [IQR 0.71-6.8 years]; Table 1). Among these, 640 (5.9%) had any ED return visit, and 290 (2.7%) had a return visit leading to admission. There was a strong left skew with minimum O2 saturation, with only 34 (0.3%) having an O2 saturation < 90%. O2 saturation was similar for encounters without return visit (median 98%, IQR 97-99%) vs those with return visit (median 98%, IQR 96-99%; p=0.07). When using an outcome of return leading to admission, there was again substantial overlap (median 98%, IQR 97-99% without return admission; median 97% IQR 96-99% with return admission), with significant difference between the two (p < 0.001). Regression models demonstrated a “U” shaped association between minimum O2 saturation and study outcomes (Figure 1). At any threshold value of O2 saturation, there were substantial compromises between sensitivity and specificity for predicting return visits (Table 2).
Conclusion(s): While a lower O2 saturation was associated with greater probability of return visit, no minimum cutoff demonstrated sufficient performance to facilitate discharge decision-making in the ED. Further research is required to identify clinical parameters maximally associated with safe discharge among children evaluated in the ED with a respiratory illness.
Table 1
.png) Sample Demographics
Sample Demographics* Total number of diagnoses exceeds the total number of cases due to multiple respiratory illness diagnoses listed for some encounters
Table 2
.png) Sensitivity, specificity, and positive likelihood ratio of minimum O2 saturation with study outcomes. Abbreviations: Sens (Sensitivity), Spec (Specificity), PLR (positive likelihood ratio), CI (Confidence Interval).
Sensitivity, specificity, and positive likelihood ratio of minimum O2 saturation with study outcomes. Abbreviations: Sens (Sensitivity), Spec (Specificity), PLR (positive likelihood ratio), CI (Confidence Interval). Figure 1
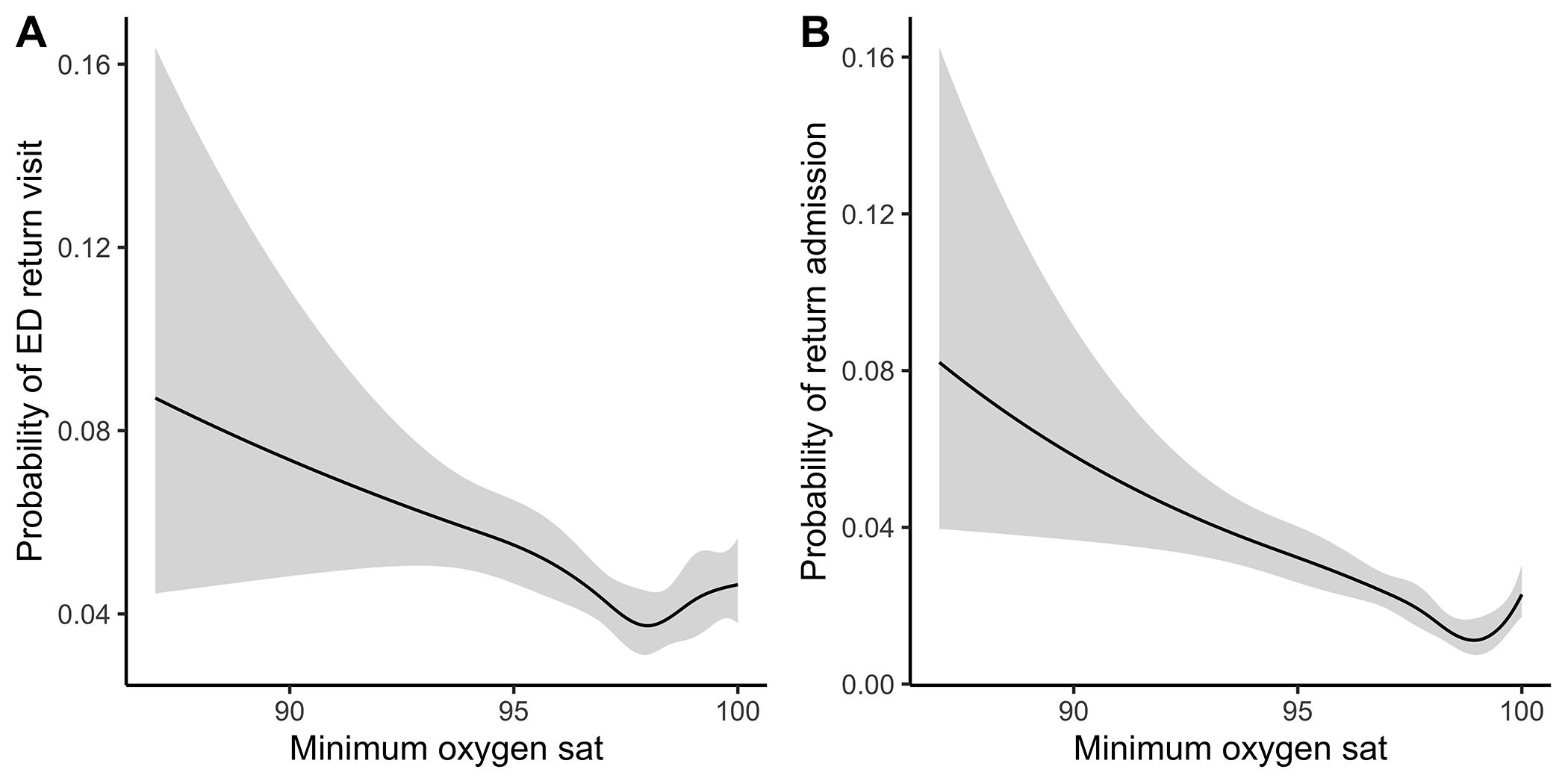 Association of minimum oxygen saturation with study outcomes in splined regression models.
Association of minimum oxygen saturation with study outcomes in splined regression models.Table 1
.png) Sample Demographics
Sample Demographics* Total number of diagnoses exceeds the total number of cases due to multiple respiratory illness diagnoses listed for some encounters
Table 2
.png) Sensitivity, specificity, and positive likelihood ratio of minimum O2 saturation with study outcomes. Abbreviations: Sens (Sensitivity), Spec (Specificity), PLR (positive likelihood ratio), CI (Confidence Interval).
Sensitivity, specificity, and positive likelihood ratio of minimum O2 saturation with study outcomes. Abbreviations: Sens (Sensitivity), Spec (Specificity), PLR (positive likelihood ratio), CI (Confidence Interval). Figure 1
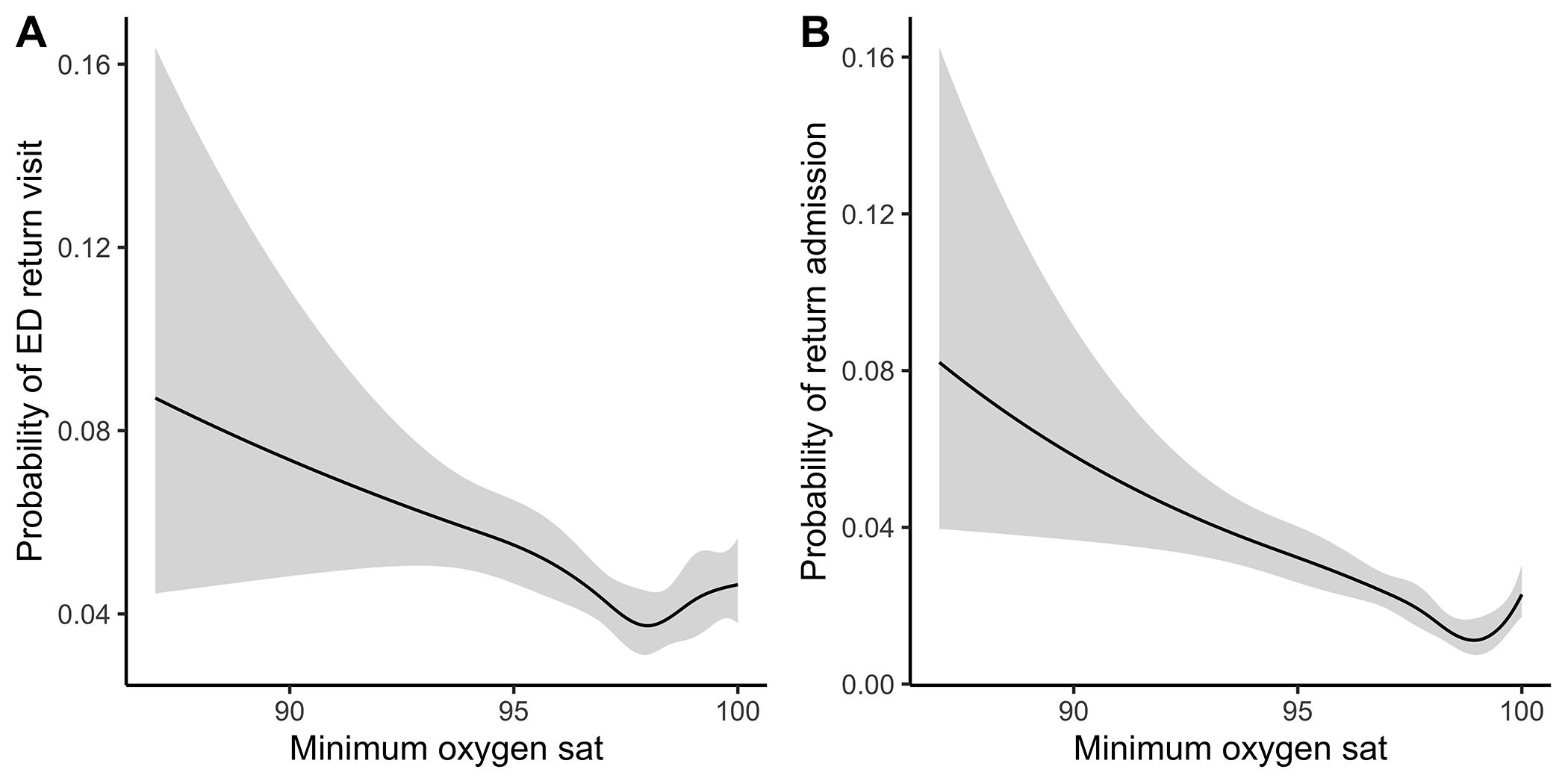 Association of minimum oxygen saturation with study outcomes in splined regression models.
Association of minimum oxygen saturation with study outcomes in splined regression models.
