Obesity 2
Session: Obesity 2
290 - Pediatric Providers' Views of the 2023 AAP Obesity Guidelines
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 290.6148
Elizabeth Kinsella, Children's Hospital Colorado, Denver, CO, United States; Courtney E. Batt, UH Rainbow Babies & Children's Hospital, Shaker Heights, OH, United States; Jeanelle Sheeder, University of Colorado School of Medicine, Aurora, CO, United States; Jaime M. Moore, University of Colorado School of Medicine, Auora, CO, United States

Jaime M. Moore, MD MPH (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Auora, Colorado, United States
Presenting Author(s)
Background: In 2023, the AAP released its first-ever Clinical Practice Guideline for obesity, which recommends earlier use of weight-loss medication (WLM) and metabolic bariatric surgery (MBS) for adolescents, in combination with lifestyle. Views of pediatric primary care providers (pPCPs) are unknown.
Objective: To describe pPCPs’ perceptions of the Guideline with a focus on WLM and MBS.
Design/Methods: An anonymous online survey sent in October 2024 via listserv to 4 pediatric primary care groups in Colorado assessed knowledge, beliefs, behaviors, and demographics of pPCPs. Descriptive and bivariate statistics were conducted. A score of >50 (0-100 scale) for a question addressing overall impact on adolescents was considered favorable.
Results: 79 providers completed the survey (72% physicians, 51% community/FQHC-based). 79% had heard about the guidelines, most (53%) from lectures, and 33% had personally reviewed them. When asked how Key Action Statements 12 and 13 (addressing WLM and MBS) would impact adolescents with obesity: 72% believed they would benefit adolescents with obesity but many reported that they would increase weight stigma (47%), disordered eating (59%), and disparities in treatment access (62%). 60% thought that mental health would improve, and 49% felt that body image would improve. 95% indicated obesity-related comorbidities would decrease.
Prior to and since guideline release, 5% of respondents performed 26+ hours/year/patient of intensive health behavior and lifestyle treatment (IHBLT) and 95% referred adolescents to weight management clinics. Prescribing WLMs increased for adolescents (11% to 27%, p< 0.001), while MBS referrals decreased slightly (33% to 30% for adolescents, p=0.002).
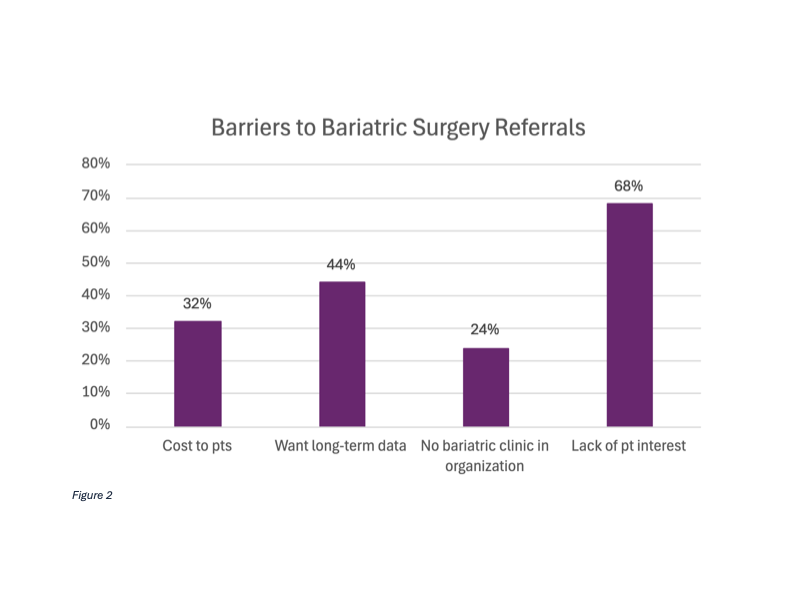
Respondents reported various barriers to prescribing WLMs and referring to MBS, as shown in Figures 1 and 2. There was no difference in prescribing or referral behaviors between those who viewed the Guideline favorably vs those who did not. Those with favorable views of the Guideline were less likely to report desire for long-term data as a barrier to prescribing WLMs (p=0.01) and referring to MBS (p=0.009).
Conclusion(s): While nearly all pPCPs believe obesity-related comorbidities will decrease in the setting of WLM and MBS recommendations, there are concerns about weight stigma, eating disorders, and equitable access, which require further study. Interventions to improve Guideline adoption should be multifaceted, targeting pPCP education, support to deliver IHBLT, adolescent beliefs, and systemic barriers such as cost and access.
Figure 1
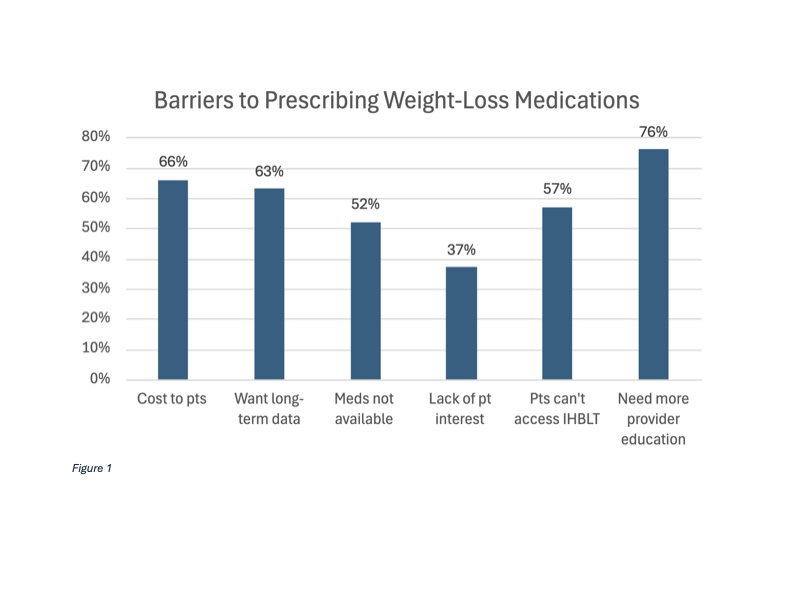
Figure 2
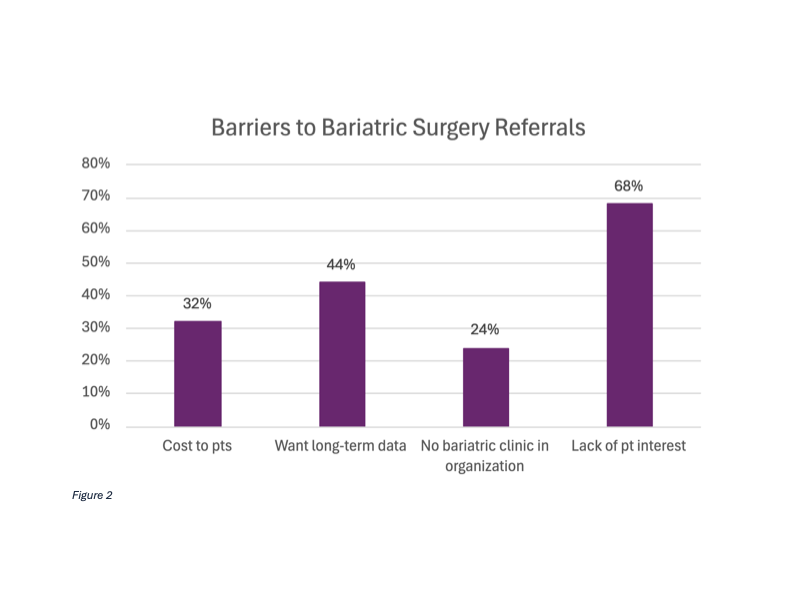
Figure 1
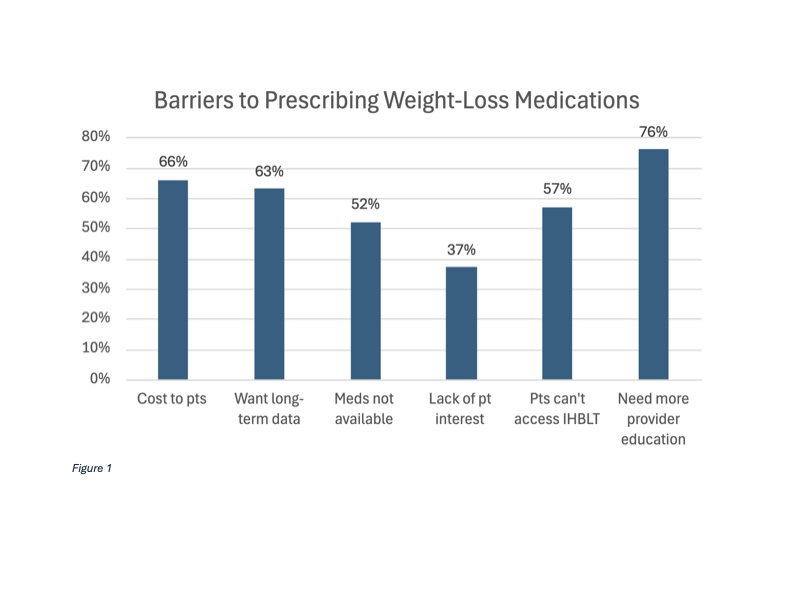
Figure 2