Children with Chronic Conditions 2
Session: Children with Chronic Conditions 2
516 - Prioritized Competencies of Pediatricians in the Care of Children with Medical Complexity: Consensus of Clinicians, Patients and Families
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 516.6359
Catherine Diskin, The Hospital for Sick Children, Toronto, ON, Canada; Naomi Gryfe Saperia, The Hospital for Sick Children, Toronto, ON, Canada; Cara L. Coleman, UVA School of Medicine INOVA Campus, Lorton, VA, United States; Bayley Levy, The Hospital for Sick Children, Toronto, ON, Canada; Kathleen Huth, Boston Children's Hospital / Harvard Medical School, Boston, MA, United States

Kathleen Huth, MD MMSc
Assistant Professor of Pediatrics
Boston Children's Hospital / Harvard Medical School
Boston, Massachusetts, United States
Presenting Author(s)
Background: Essential competencies of pediatricians who provide high-quality care for children with medical complexity (CMC) must be defined to design educational programs to achieve the desired outcome. Patients and families are key stakeholders in defining these competencies.
Objective: To identify high-priority competencies of all pediatricians in the care of CMC, reflecting the consensus of clinicians, family caregivers and young adults with medical complexity.
Design/Methods: We used consensus development methodology guided by a steering committee of complex care clinicians, researchers, and family leaders. We recruited participants via an international complex care listserv, family-led organizations and social media, using purposeful sampling to ensure a range of clinical and lived experience in the care of CMC. In Round 1, participants responded to an open-ended prompt about competencies of pediatricians who care for CMC. After refinement of responses by the steering committee, participants rated the importance of each competency using a 7-point Likert scale (Round 2). In Round 3, participants rated the importance of the top ranked competencies from Round 2 and identified 10 essential competencies.
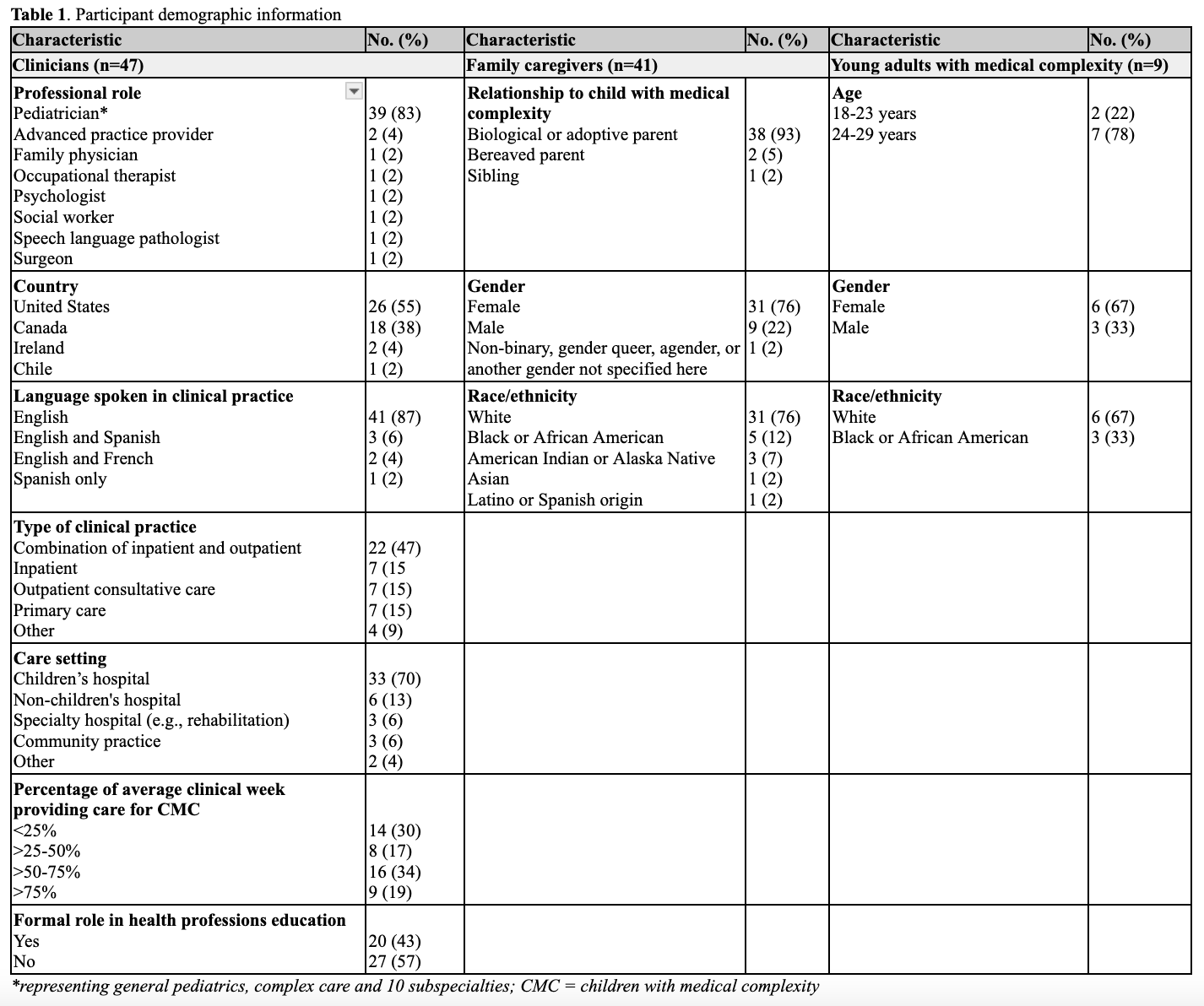
Results: From March-July 2024, a diverse expert panel consisting of 47 clinicians, 41 family caregivers and 9 young adults with medical complexity participated (Table 1); 71 of the 97 participants completed all 3 rounds (73%). In Round 1, 131 responses were synthesized into 94 competencies in 5 domains: medical expertise, collaborative care, patient- and family-centered care, partnership in advocacy, and reflective practice. In Round 2, 38 of the 94 competencies were prioritized as very important for all pediatricians in the care of CMC. In Round 3, top identified competencies beyond medical expertise included: values the whole child and demonstrates a humanistic approach to care, demonstrates integrity in clinical practice, collaborates with an interprofessional team outside of healthcare, engages in shared decision-making, recognizes the impact of systemic factors on the family experience, demonstrates curiosity and flexibility, appreciates uncertainty, and recognizes the importance of care coordination.
Conclusion(s): An international expert panel of clinicians, patients and families identified high-priority competencies for all pediatricians in the care for CMC. These findings can be used to advance a collaborative postgraduate education agenda that reflects the perspectives of all stakeholders to support optimal care for CMC.
Table 1: Participant demographic information