Infectious Diseases 6: Infectious diseases syndromes
Session: Infectious Diseases 6: Infectious diseases syndromes
057 - Pilonidal abscesses: microbiologic characteristics and antimicrobial treatment options
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 57.6440
David Sebastian Garcia, The University of Toledo College of Medicine and Life Sciences, Toledo, OH, United States; Joshua R. Watson, Nationwide Children's Hospital, Columbus, OH, United States; Guliz Erdem, Nationwide Children's Hospital, columbus, OH, United States
- DG
David Sebastian Garcia, n/a (he/him/his)
The University of Toledo College of Medicine and Life Sciences
Toledo, Ohio, United States
Presenting Author(s)
Background: Pilonidal abscesses (PA), commonly seen in adolescents, occur due to inflammation from debris stuck under the skin of the gluteal cleft. In many patients it becomes a chronic, recurring disease. However, there is a paucity of published data regarding the microbiology of PAs to guide empiric antibiotic treatment.
Objective: To define the causative organisms in recurrent PAs and inform antimicrobial treatment decisions.
Design/Methods: We reviewed the EMR of children aged ≤18 years hospitalized with a diagnosis of “pilonidal abscess” or “pilonidal cyst” who had operating room wound cultures between October 1, 2014 and October 1, 2024. Encounters were classified as recurrent if there was a previous encounter of PA, or if a prior PA was indicated in the patient’s problem list or past medical history. Pretreatment referred to any antibiotics administered during the encounter prior to the operating room cultures.
Results: A total of 109 aerobic and anaerobic samples were obtained from 81 patients. There were 47 patients who had recurrent PA. At least one microorganism was recovered from 95 aerobic and 84 anaerobic cultures. Overall, Peptostreptococcus spp, S. anginosus, and Bacteroides spp. were the most common microorganisms identified. Prevotella spp., coagulase-negative staphylococci (CoNS), and Peptostreptococcus spp. were most frequently recovered from recurrent abscesses (Table 1). Only 1 culture yielded methicillin-resistant Staphylococcus aureus (MRSA).
A single microorganism was identified in 17% of aerobic cultures and 6% of anaerobic cultures. S. anginosus, CoNS, and Actinomyces were the most common single microorganism isolates.
Clindamycin and ampicillin-sulbactam (A/S) were the most prescribed antibiotics prior to surgery (Table 2). Ten patients did not receive pretreatment. Among those treated with clindamycin, 94% of aerobic cultures and 78% of anaerobic cultures had microorganism growth. 80% of aerobic and anaerobic cultures had bacterial growth in patients pretreated with A/S.
Conclusion(s): Anaerobes, S. anginosus, CoNS, Actinomyces spp., and enteric Gram-negative rods were most frequently isolated from PAs, including recurrent PAs. The pathologic role of CoNS in PAs is unclear. MRSA was rarely isolated. Based on the microbiology, if empiric antibiotic therapy is deemed necessary, A/S or amoxicillin/clavulanate is the optimal choice.
Table 1. Microorganisms identified from all pilonidal abscesses and from recurrent abscesses.
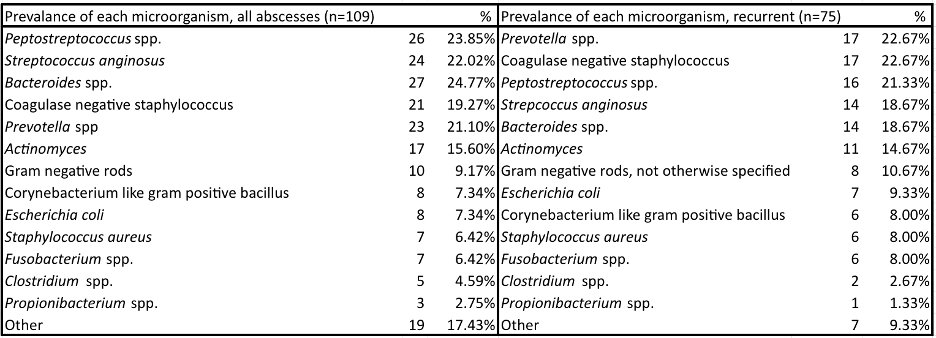
Table 2. Microorganisms identified based off antibiotic pretreatment.
.png)

