Children with Chronic Conditions 2
Session: Children with Chronic Conditions 2
515 - Persistence and reappearance of tracheostomy aspirate Pseudomonas after antipseudomonal antibiotic use
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 515.6489
Elaina Schueler, Medical College of Wisconsin, Milwaukee, WI, United States; Jennifer Henningfeld, Medical College of Wisconsin, Milwaukee, WI, United States; Rebecca Steuart, Medical College of Wisconsin, Milwaukee, WI, United States
- ES
Elaina Schueler, BA (she/her/hers)
Clinical Research Coordinator
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Pseudomonas aeruginosa (Ps) is frequently identified in respiratory cultures from children with tracheostomies and is often targeted with antipseudomonal antibiotics (antiPs). The clearance vs. persistence of Ps on cultures following antiPs exposure is not well described.
Objective: To identify the frequency of Ps identification in tracheostomy aspirate(TA) cultures before and after antiPs exposure, and the time until Ps reappears following treatment.
Design/Methods: This longitudinal prospective study enrolled infants 2-12 months old undergoing new tracheostomy placement. TA samples were collected at tracheostomy placement, during illness, and quarterly during wellness. Samples underwent bacterial culture and organism identification per routine microbiology lab protocols. TA culture results prior to tracheostomy placement and all prescribed antiPs were obtained from the medical record. Each culture was categorized based on Ps status in relation to prior cultures: initial identification, persistent presence, disappearance, persistent absence, or reappearance. For each culture with Ps status change, Ps presence and timing since last antiPs dose were determined. If no prior antiPs, the child’s age in days was used.
Results: We analyzed 121 TA cultures obtained from 7 children(median 18 per child, IQR:12-23; 60% during illness) over median follow up of 19.9 months(10.7-24.1). Children were median 3.5 mo at tracheostomy placement and 5 had chronic ventilator use(Table 1). Children received a total of 25 antiPs courses(median 3 per child, IQR:2-5), most frequently cefepime and tobramycin nebulization, with short durations (median 2.5 days, IQR:1-5). In 9 instances, TA culture identified Ps within 1 week of antiPs, while 5 courses followed a positive Ps culture within 3 months.
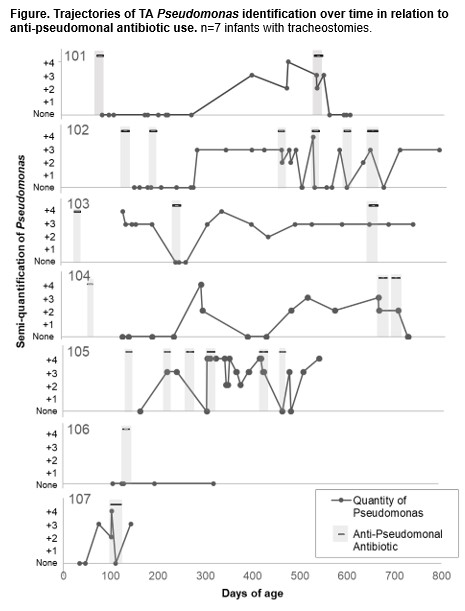
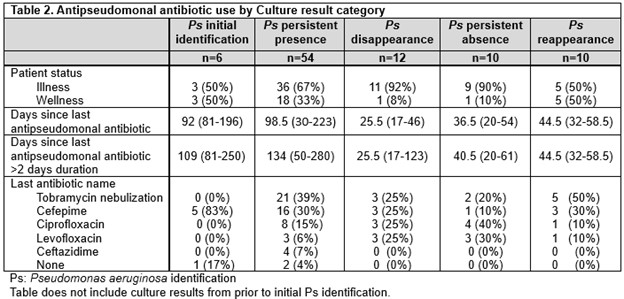
There were 28 Ps status changes: 6 initial identifications, 12 disappearances, and 10 reappearances.(Table 2) Initial identification occurred at median age 8.4mo(IQR:5.0-9.7) and median 3.4 months after tracheostomy placement (IQR:1.6-5.5). Ps disappeared a median 25.5 days(17-46) after last antiPs use. Ps reappeared in 10/12(83%) instances at median 44.5 days after last antiPs exposure(IQR:32-58.5). In 3 instances, Ps disappeared without corresponding antiPs exposure within 7 days. In 4 instances, Ps persisted despite antiPs exposure (Figure).
Conclusion(s): Although short courses of antiPs antibiotics transiently eliminated Ps in TA cultures, the effect was short-lived with frequent recurrence. There may be limited benefit to targeting Ps for long-term eradication in infants with tracheostomies.
Table 1
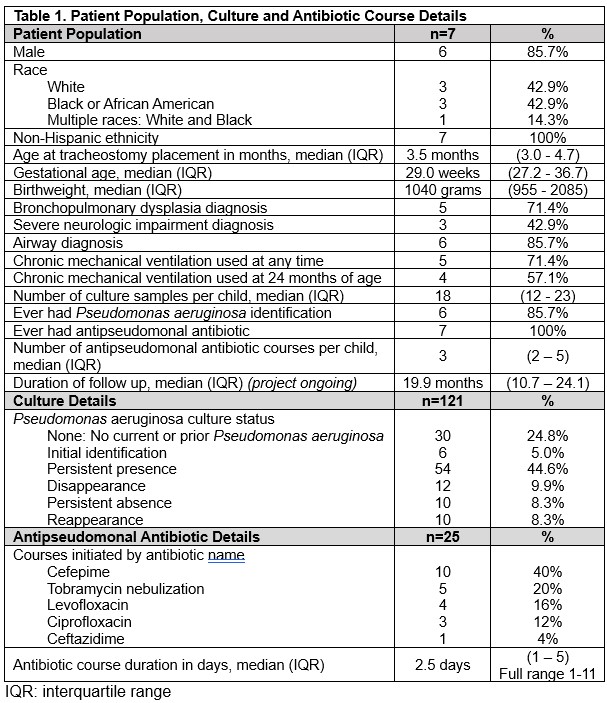
Table 2
Trajectories of TA Pseudomonas identification over time in relation to anti-pseudomonal antibiotic use. n=7 infants with tracheostomies.