Hospital Medicine 4: Medical Education
Session: Hospital Medicine 4: Medical Education
166 - The Mentor’s Lens: Assessing Personal Growth Through Structured Mentorship
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 166.6553
Sandra Gage, Phoenix Children's Hospital, Racine, WI, United States; Vasudha L.. Bhavaraju, University of Arizona College of Medicine - Phoenix, Phoenix, AZ, United States; Reina Patel, Phoenix Children's Hospital, Phoenix, AZ, United States
.jpg)
Reina Patel, DO, FAAP (she/her/hers)
Associate Clinical Professor, Child Health
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Mentorship has been shown to improve professional satisfaction and career growth for mentees and is important in the development of faculty at all levels, but little has been published about methods for preparing mentors to succeed in this vital role. Literature is also scarce on mentor benefits of mentorship participation. To investigate these factors, we implemented a structured mentorship program for our pediatric hospital medicine (PHM) faculty.
Objective: Determine the impact of a structured mentorship program on PHM faculty mentors’ professional satisfaction and perceived mentor qualities and skills.
Design/Methods: We conducted an interventional pilot study in our PHM division from 1/2021-1/2024. Experienced PHM members were asked to participate voluntarily as mentors. Accepting mentors completed a pre-survey to aid in mentee matching. Mentorship program leadership provided a joint mentor/mentee session and 2 mentor only sessions related to goal development and strategies/skills for successful mentorship. Each pair met bimonthly for 1 year using a structured format; program leadership performed 2 formal check-ins. Mentors completed a post-program survey consisting of 5-point Likert scale and open-ended questions. We used descriptive statistics to analyze results; open-end question comments were reviewed to clarify key points.
Results: Nine mentor surveys were completed in 3 program cycles. On a scale from 1-5 (1=None; 5=Great Degree), mean responses for mentor perception of program impact on mentor qualities ranged from 3.44 to 4.44 with most program attributable improvement in listening and empowering; least in directness (Fig 1). Mean responses for improvement to mentor skills ranged from 3.67 to 4.1, with most program attributable improvement in promotion of leadership and networking; least in clinical excellence (Fig 2). Most mentors strongly agreed that participation led to increased professional satisfaction (Mean score 4.78). Open-ended responses regarding the most successful part of the program highlighted themes of personal satisfaction from helping to advance colleague professional progress and development of mentor skills.
Conclusion(s): Our study demonstrates that participation in a structured mentorship program can increase PHM mentors’ perceived abilities in both key mentor qualities and skills, while improving professional satisfaction for most. The benefit of programs of this type can have far-reaching effects for any field. Future efforts will target improving mentor educational support for key qualities and skills with the lowest improvement scores.
Mentor Qualities
.png) Fig. 1. Mean perceived improvement in mentor qualities due to program participation.
Fig. 1. Mean perceived improvement in mentor qualities due to program participation. Mentor Skills
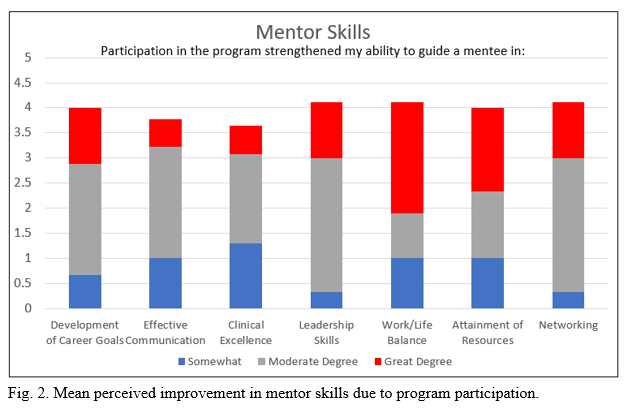 Fig. 2. Mean perceived improvement in mentor skills due to program participation.
Fig. 2. Mean perceived improvement in mentor skills due to program participation. Mentor Qualities
.png) Fig. 1. Mean perceived improvement in mentor qualities due to program participation.
Fig. 1. Mean perceived improvement in mentor qualities due to program participation. Mentor Skills
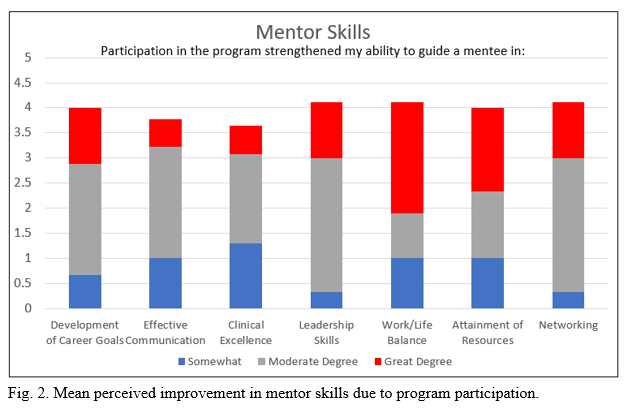 Fig. 2. Mean perceived improvement in mentor skills due to program participation.
Fig. 2. Mean perceived improvement in mentor skills due to program participation. 
