Hospital Medicine 5: Clinical
Session: Hospital Medicine 5: Clinical
531 - Tick Tock, Beep Boop: Daily Temporal Trends in Clinical Alarm Rates
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 531.6574
Nicholas Clark, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Katina L. Rahe, The Children's Mercy Hospital, HCO-ID 8347 (Kansas City, MO), Prairie Village, KS, United States; Ginny M. Nyberg, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Lindsey Malloy-Walton, Children`s Mercy Hospital, Kansas City, MO, United States; Kathryn E. Kyler, Children's Mercy Kansas City, Kansas City, MO, United States; Matthew Hall, Children's Hospital Association, Lenexa, KS, United States; Christine Claeys, Children's Mercy, Kansas City, MO, United States; Kathleen J. Berg, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Geoffrey L. Allen, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States

Nicholas Clark, MD
Associate Professor of Pediatrics
Children's Mercy Kansas City
Kansas City, Missouri, United States
Presenting Author(s)
Background: Frequent inpatient clinical alarm exposure leads to alarm fatigue and missed patient decompensation. Identifying the hours in which alarms are more frequent would aid in implementation of alarm stewardship practices and highlight times in which patients may be at increased risk for unrecognized clinical deterioration. However, daily temporal trends in clinical alarm rates remains unknown.
Objective: We aimed to describe alarm rate trends by hour of the day and compare daytime (07:00-18:59) versus nighttime (19:00-06:59) alarm rates.
Design/Methods: We conducted a retrospective study of clinical alarm and patient census data at a freestanding children’s hospital from 1/1/2023-12/31/2023, including 10 inpatient units: 8 medical/surgical (MSU), 1 pediatric intensive care unit (PICU), and 1 cardiac intensive care unit (CICU). Alarm rates per patient day per hour-of-day were calculated. Hour-of-day alarm rates were stratified by unit type (i.e., MSU, PICU, and CICU), alarm source (e.g., pulse oximetry), and cause (e.g., low oxygen saturation). Poisson regression was used to determine p-values for comparisons.
Results: There were 3,274,872 alarms included across 54,558 patient days. The overall rate was 60 alarms per patient day (95% confidence interval [CI]: 60-60.1; MSU 57.6 vs PICU 62.8 vs CICU 78.1; p<.001). Hour-of-day alarm rates varied (range 40.3 at 01:00 to 85.8 at 20:00) with major peaks occurring at 08:00 and 20:00 and minor peaks at 00:00, 04:00, 12:00, 16:00 (Figure 1). Similar peaks occurred across nearly all unit types, alarm sources, and causes (Figures 1&2). Alarm classifications displaying the most prominent peaks were ‘pulse oximetry’ for alarm sources and ‘technical’ for alarm causes (Figure 2). Overall, daytime hours had significantly higher rates of alarms than nighttime hours (66.8 [95%CI 66.7-66.9] vs 53.2 [95%CI 53.1-53.3]; p<.001). Across all unit types, alarm sources, and causes, daytime alarm rates were also significantly higher than nighttime, except for ‘low heart rate’ which had a significantly higher nighttime vs daytime alarm rate (6.4 [95%CI 6.3-6.4] vs 3.7 [95%CI 3.7-3.7]; p<.001; Table).
Conclusion(s): Daily temporal trends in clinical alarms existed at our institution in 2023, with higher alarm rates occurring during daytime versus nighttime hours for nearly all characteristics studied. Alarm rate peaks clustered around hours of initial patient assessments during nursing unit shift changes and during hours of routine vital sign assessments. Alarm stewardship opportunities, particularly for pulse oximetry and technical alarms, likely exist during hours of peak alarm rates.
Figure 1. Alarm Rates Across the 24-Hour Day.
.jpg) Data presented overall and stratified by unit type.
Data presented overall and stratified by unit type.CICU, cardiac intensive care unit. MSU, 8 medical/surgical units combined. PICU, pediatric intensive care unit.
Figure 2a. Alarm Rates Across the 24-Hour Day: By Alarm Sources. Figure 2b. Alarm Rates Across the 24-Hour Day: By Alarm Causes.
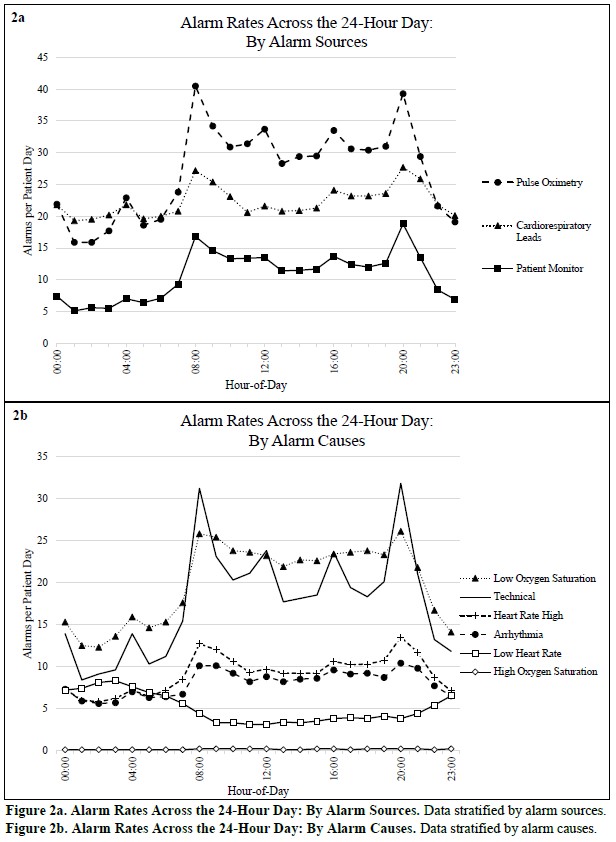 2a, Data stratified by alarm sources. 2b, Data stratified by alarm causes.
2a, Data stratified by alarm sources. 2b, Data stratified by alarm causes.Table. Daytime versus Nighttime Alarm Rates.
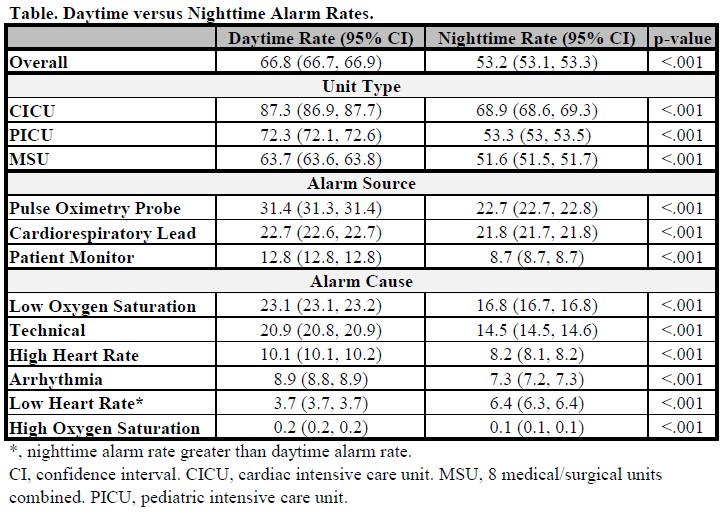 *, nighttime alarm rate greater than daytime alarm rate.
*, nighttime alarm rate greater than daytime alarm rate.CI, confidence interval. CICU, cardiac intensive care unit. MSU, 8 medical/surgical units combined. PICU, pediatric intensive care unit.
Figure 1. Alarm Rates Across the 24-Hour Day.
.jpg) Data presented overall and stratified by unit type.
Data presented overall and stratified by unit type.CICU, cardiac intensive care unit. MSU, 8 medical/surgical units combined. PICU, pediatric intensive care unit.
Figure 2a. Alarm Rates Across the 24-Hour Day: By Alarm Sources. Figure 2b. Alarm Rates Across the 24-Hour Day: By Alarm Causes.
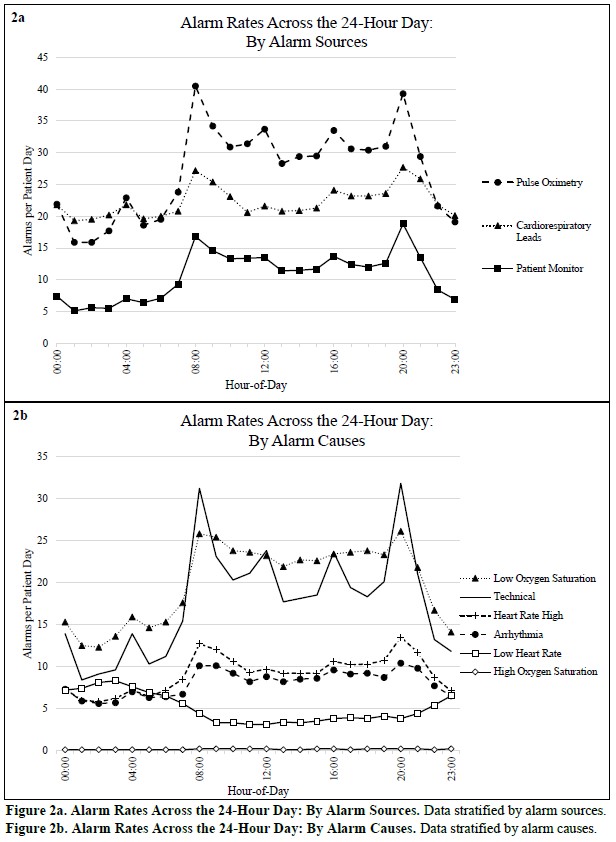 2a, Data stratified by alarm sources. 2b, Data stratified by alarm causes.
2a, Data stratified by alarm sources. 2b, Data stratified by alarm causes.Table. Daytime versus Nighttime Alarm Rates.
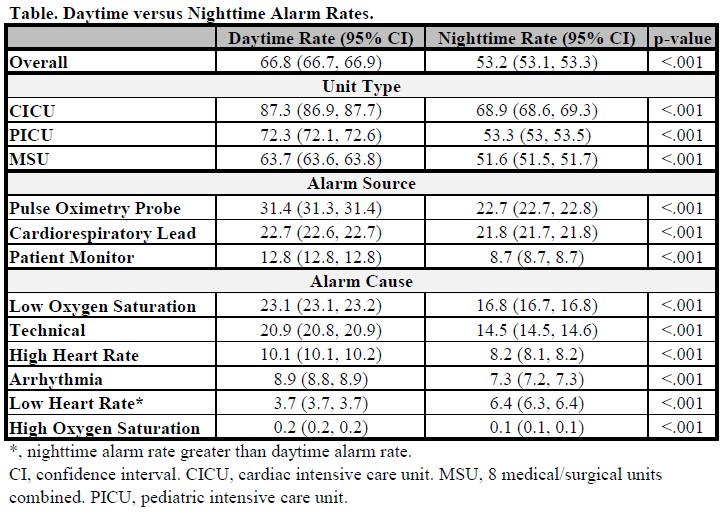 *, nighttime alarm rate greater than daytime alarm rate.
*, nighttime alarm rate greater than daytime alarm rate.CI, confidence interval. CICU, cardiac intensive care unit. MSU, 8 medical/surgical units combined. PICU, pediatric intensive care unit.

