Health Equity/Social Determinants of Health 6
Session: Health Equity/Social Determinants of Health 6
734 - Social Needs Screening and Uptake Patterns of a Produce Prescription Program in an Urban Pediatric Primary Care Clinic
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 734.6724
Claire E.. Branley, UMass Chan Medical School, Worcester, MA, United States; Maya B D. O'Connor, UMass Memorial Children's Medical Center, Salem, MA, United States; Leela Garg, UMass Memorial Children's Medical Center, Newtonville, MA, United States; Alison LeBlanc, Self, East Boston, MA, United States; Katherine Barahona Paz, Boston Children's Hospital, Cambridge, MA, United States; Arvin Garg, UMass Memorial Children's Medical Center, Worcester, MA, United States; Stephenie C. Lemon, UMass Chan Medical School, Worcester, MA, United States

Claire E. Branley, BS (she/her/hers)
MD/PhD Candidate
UMass Chan Medical School
Worcester, Massachusetts, United States
Presenting Author(s)
Background: In 2023, approximately 1 in every 11 households with children in the US were food insecure, which has negative implications for children’s health and development. Social needs screening and referral systems have been implemented in pediatric primary care settings nationally to address food insecurity and other social determinants of health. However, it remains unknown whether caregiver’s responses to these screeners correlate with acceptance of assistance.
Objective: We evaluated screening data from an urban pediatric clinic and the uptake of Fresh Connect (FC), which provides families $80 per month for fresh fruits and vegetables for 6 months. Our aim is to determine whether screening positive for wanting help with food increased the odds of enrollment in FC.
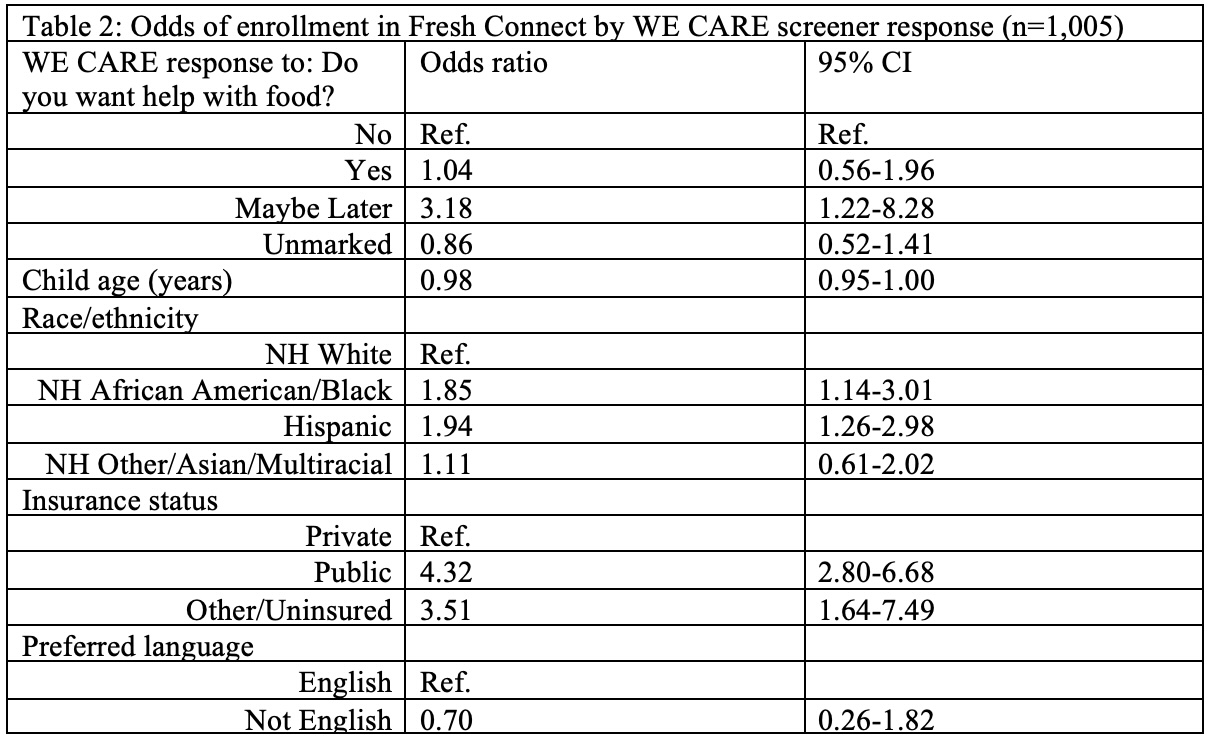
Design/Methods: The WE CARE screening system, a self-report instrument for 8 social needs, was implemented in an urban pediatric clinic beginning in October 2021. Families who completed a screener (n=1049) and spoke English, Spanish, or Portuguese were followed-up via telephone offered FC regardless of screener results. Child age, race/ethnicity, caregiver’s preferred language, and insurance were extracted from their medical record. Cases with missing sociodemographic data (n=44) were removed for a final sample of n=1,005. A multivariable adjusted logistic regression model was utilized to describe the association between WE CARE responses and enrolling in FC.
Results: Overall, 38% of the children sample were of NH White race/ethnicity; 97% of caregivers spoke English, and the majority (52%) were on public insurance. Among caregivers who completed the WE CARE screener, 78% did not request help with food, while 6% said yes and 2% said “maybe later”; 14% left the question blank. Overall, 20% enrolled in FC (n=202). Indicating “yes” to needing help with food did not increase odds of FC enrollment after controlling for demographic characteristics. Choosing “maybe later” was associated with 3.2 higher odds of FC enrollment (95% CI 1.2-8.3).
Conclusion(s): Caregivers were accepting of pediatric produce prescription regardless of indicated food need. Reporting wanting help with food “maybe later” on the WE CARE screener was significantly associated with FC enrollment; surprisingly, responding “yes” was not. This study is the first to explore concordance between screening responses and a food is medicine intervention enrollment. Future primary care-based interventions should evaluate the role of social needs screeners in the referral pathway and consider, when possible, offering food-related assistance to all families regardless of screening responses.
Table 1: Sample sociodemographic characteristics, by parental report of desiring assistance with food on the WE CARE screener (n=1,005)
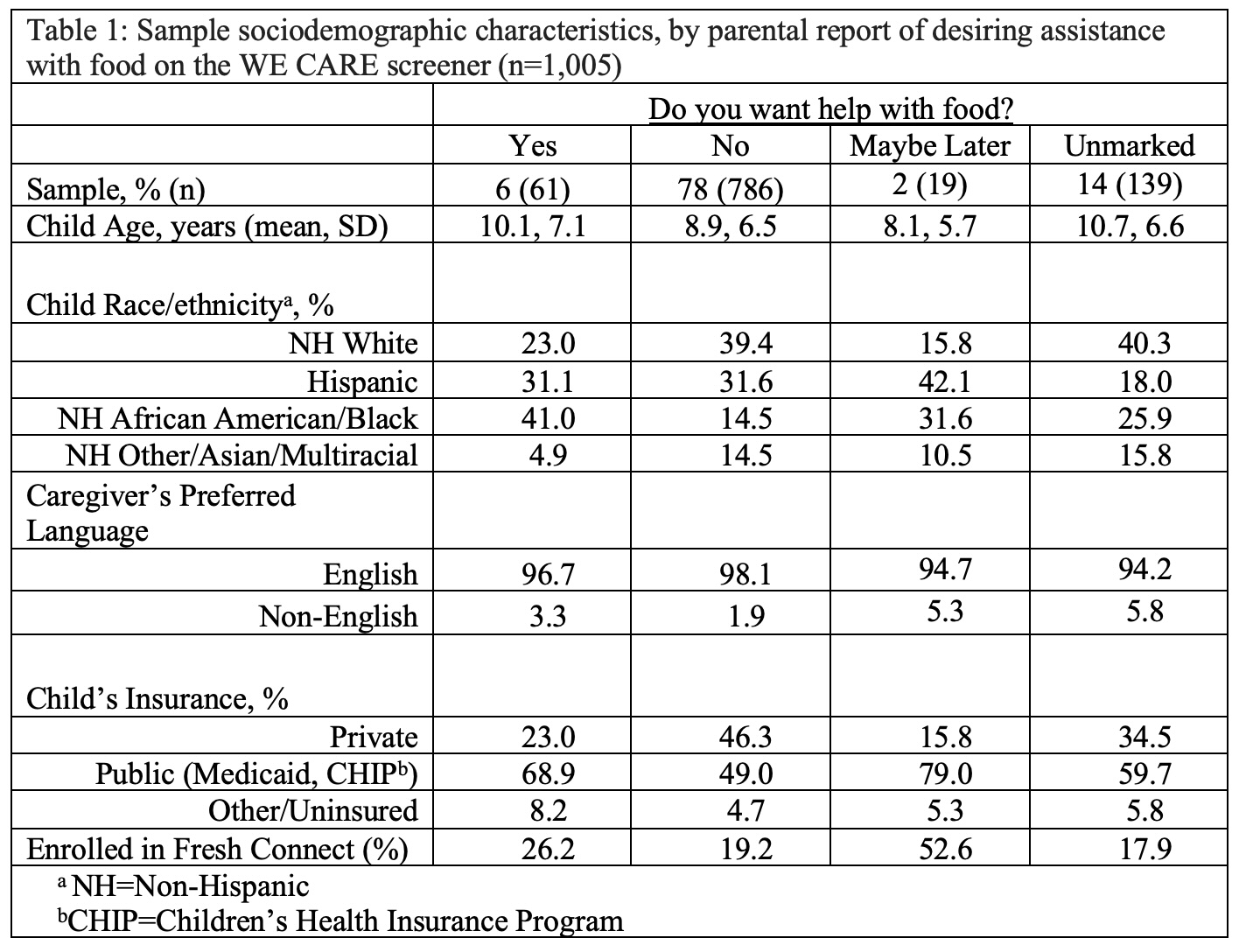
Table 2: Odds of enrollment in Fresh Connect by WE CARE screener response (n=1,005)