Neonatal Fetal Nutrition & Metabolism 1
Session: Neonatal Fetal Nutrition & Metabolism 1
609 - Beyond Calories: Identifying Volume-Based Nutrition Strategies to Prevent Malnutrition in Preterm Infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 609.3893
Gabriella E. Gegel, Santa Clara University, San Antonio, TX, United States; Alvaro Moreira, The University of Texas Health Science Center at San Antonio Joe R. and Teresa Lozano Long School of Medicine, San Antonio, TX, United States

Gabriella E. Gegel (she/her/hers)
Student
Santa Clara University
San Antonio, Texas, United States
Presenting Author(s)
Background: Adequate nutrition is essential for supporting optimal growth and development in premature infants, who are at increased risks of morbidity and mortality from malnutrition.
Objective: To identify early-life, modifiable risk factors related to feeding practices and clinical indicators that could reduce the likelihood of severe malnutrition in preterm infants.
Design/Methods: We conducted a retrospective analysis of 672 neonates from the University of Texas Health San Antonio (2014-2022). Infants with a birthweight z-score < -2 were excluded. We collected 100 features, including demographics, neonatal morbidity, birth anthropometrics, and nutrition data (both TPN and enteral feed intake) during the first month of life. Multiple supervised ML models were trained on data collected by day 28, with 70% for training and 30% for testing.
Results: Among the 672 infants, those with severe malnutrition (n=122, 18.2%) had significantly lower gestational ages (27.2 vs. 29.5 weeks, p< 0.001), birth weights (1,072g vs. 1,267g, p< 0.001), and birth weight z-scores (-0.55 vs. -0.19, p< 0.001) compared to the non-malnourished group. They also required more respiratory support by day 28 (76% vs. 39%, p< 0.001). Nutritional intake patterns differed notably: the severe malnutrition group received higher TPN caloric intake early on (68 kcal on day 7 vs. 60 kcal, p< 0.05) but consistently lower enteral calories, especially by day 14 (69 kcal vs. 100 kcal, p< 0.05). The Random forest model achieved the highest predictive accuracy, with an area under the curve of 92.5%, sensitivity of 60.6%, and specificity of 92.7%. Feed volume, rather than caloric density, was an important protective factor. By day 28, non-malnourished infants reached a mean feed volume of 125 mL/kg, compared to 95 mL/kg in the malnutrition group.
Odds ratio analysis reinforced feed volume as protective against severe malnutrition, with significantly lower odds of malnutrition associated with higher feed volumes on days 7, 14, and 28 (all ORs < 1), while caloric density alone was insufficient to reduce malnutrition risk.
Conclusion(s): Early enteral feed volume is a key protective factor in reducing severe malnutrition risk in preterm infants, highlighting the importance of prioritizing feed volume in neonatal nutrition strategies. These findings indicate that emphasizing early feed volume adjustments may contribute to better growth outcomes in preterm infants. Prospective validation and integration into clinical protocols are warranted.
Figure 2. Logistic Regression Analysis of Volume and Caloric Intake
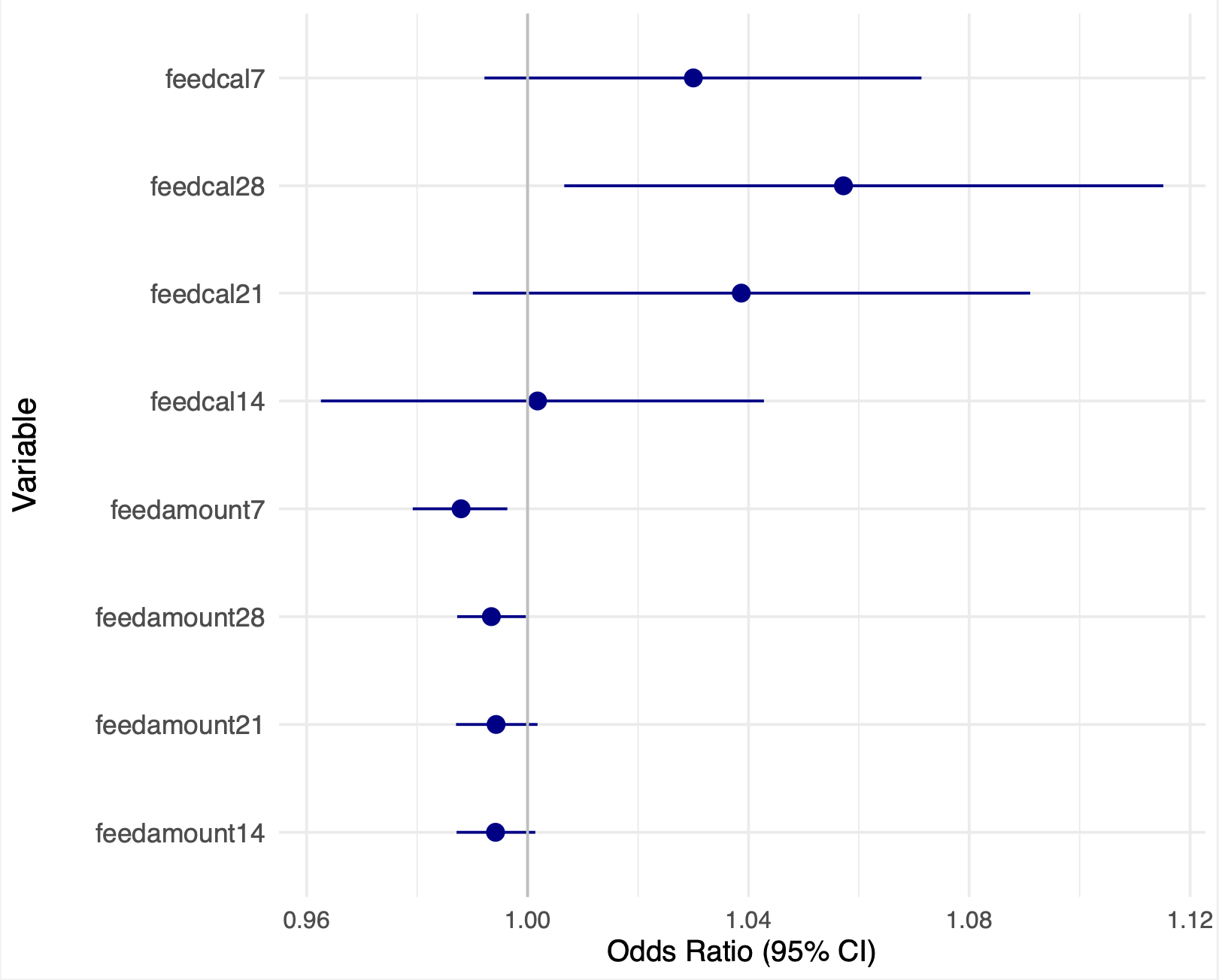
Figure 1. Volume and Caloric Intake over the First Month of Life
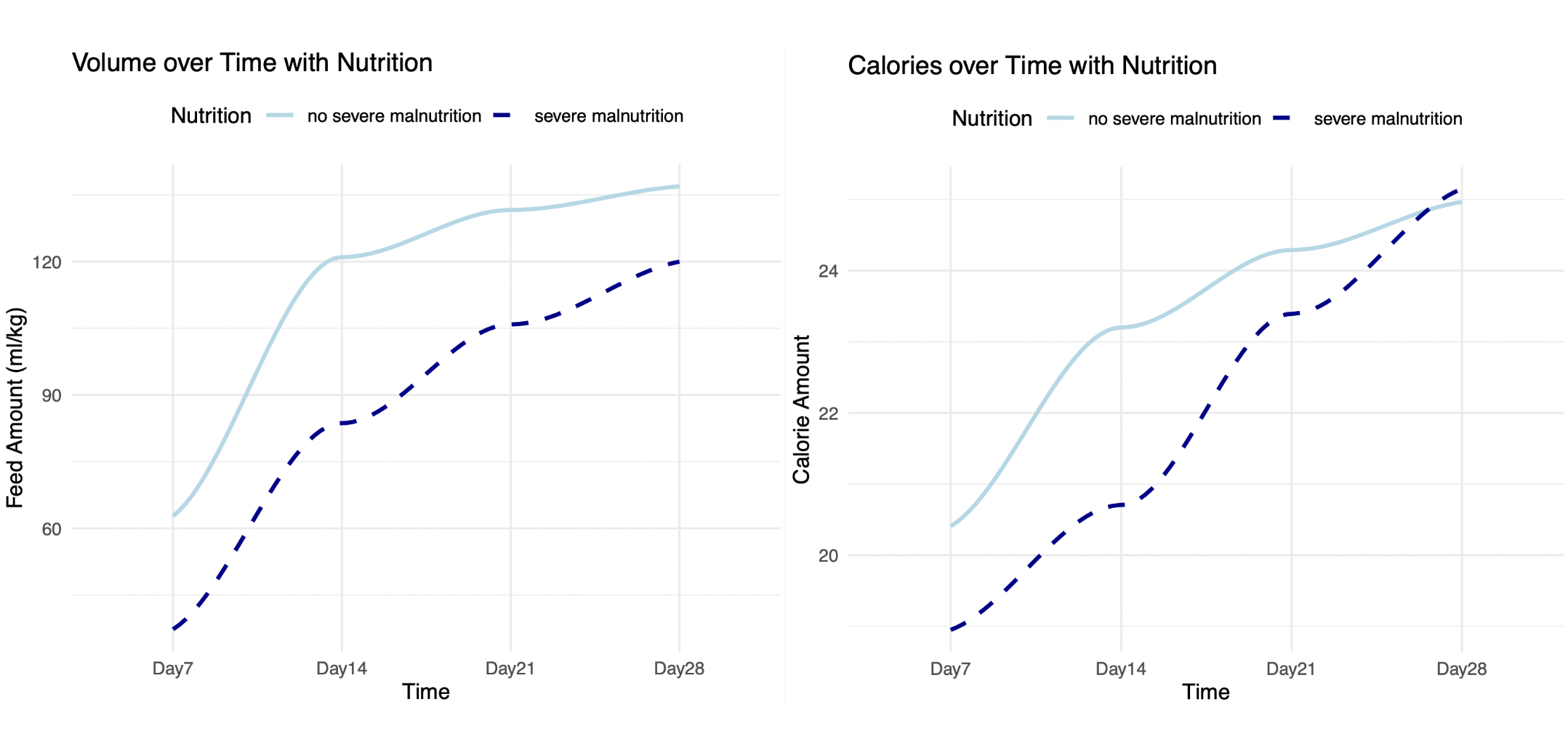
Table 1. Demographic and Nutritional Characteristics
.png)

