Breastfeeding/Human Milk 2
Session: Breastfeeding/Human Milk 2
652 - Mother’s Own Milk Feeding in Preterm Infants: A Single Center Retrospective Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 652.5755
Yohanna Tesfaye, Baylor College of Medicine, Houston, TX, United States; Jazmine Elleston, Baylor College of Medicine, Houston, TX, United States; Monika Patil, Baylor College of Medicine, Houston, TX, United States; Joseph Hagan, Baylor College of Medicine, Houston, TX, United States

Yohanna Tesfaye, MD
Resident
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Mother’s own Milk (MOM) has a multitude of health benefits for preterm infants such as decreased risk of necrotizing enterocolitis and retinopathy of prematurity, as well as improved neurodevelopmental outcomes. Studies show maternal race, age, and education level has an impact on MOM use in preterm patients. Mode of delivery and gestational age have also been shown to influence earlier MOM cessation in preterm patients. Furthermore, maternal pregnancy complications may also have an impact on use and discontinuation of MOM, but data on this in recent years is lacking.
Objective: In our center, we see a wide range of patients from varying races and socioeconomic backgrounds. We aimed to examine maternal and neonatal factors related to use of MOM among our preterm infants.
Design/Methods: This was a retrospective analysis of Vermont Oxford Network data specific to the institution and its milk bank. We included infants born < 35 weeks gestation, without major congenital anomalies, born at and admitted to the NICU between January 1, 2018 and December 31, 2022. Logistic regression analysis was used to examine the association of maternal and neonatal factors with two outcomes: infants receiving < 30% MOM and infants receiving >70% MOM. These associations were examined separately within each race and ethnic group in addition to all patients combined.
Results: The cohort included 2230 patients: 837 (37.5%) received < 30% MOM and 773 (34.7%) received >70% MOM. Over 70% MOM use was more likely in very low birthweight (VLBW, < 1500g) infants compared to those with >2500g birthweight (Odds ratio [OR] 3.74, 95% Confidence Interval [CI] 2.506, 5.582, p< 0.0001). Preterm infants on Medicaid were less likely to receive >70% MOM compared to those with commercial insurance (OR 0.457, 95% CI 0.382, 0.547, p< 0.0001). Infants of mothers with hypertension were less likely to receive >70% MOM (OR 0.739, 95% CI 0.618, 0.884, p=0.001), particularly in African American (AA) infants (OR 0.691, 95% CI 0.492, 0.969, p=0.032). Infants of diabetic mothers were less likely to receive >70% of MOM (OR 0.621, 95% CI 0.483, 0.798, p=0.0002), particularly in AA (OR 0.478, 95% CI 0.268, 0.854, p=0.0127) and Hispanic infants (OR 0.425, 95% CI 0.271, 0.667, p=0.0002).
Conclusion(s): In our cohort, VLBW infants had higher odds of receiving majority MOM. AA and Hispanic infants had lower odds of receiving majority MOM in cases with Medicaid insurance, maternal hypertension and diabetes. Identifying associations with lower odds of majority MOM use may help clinicians be more aware and ultimately address barriers to majority MOM use in these groups.
Figure 1
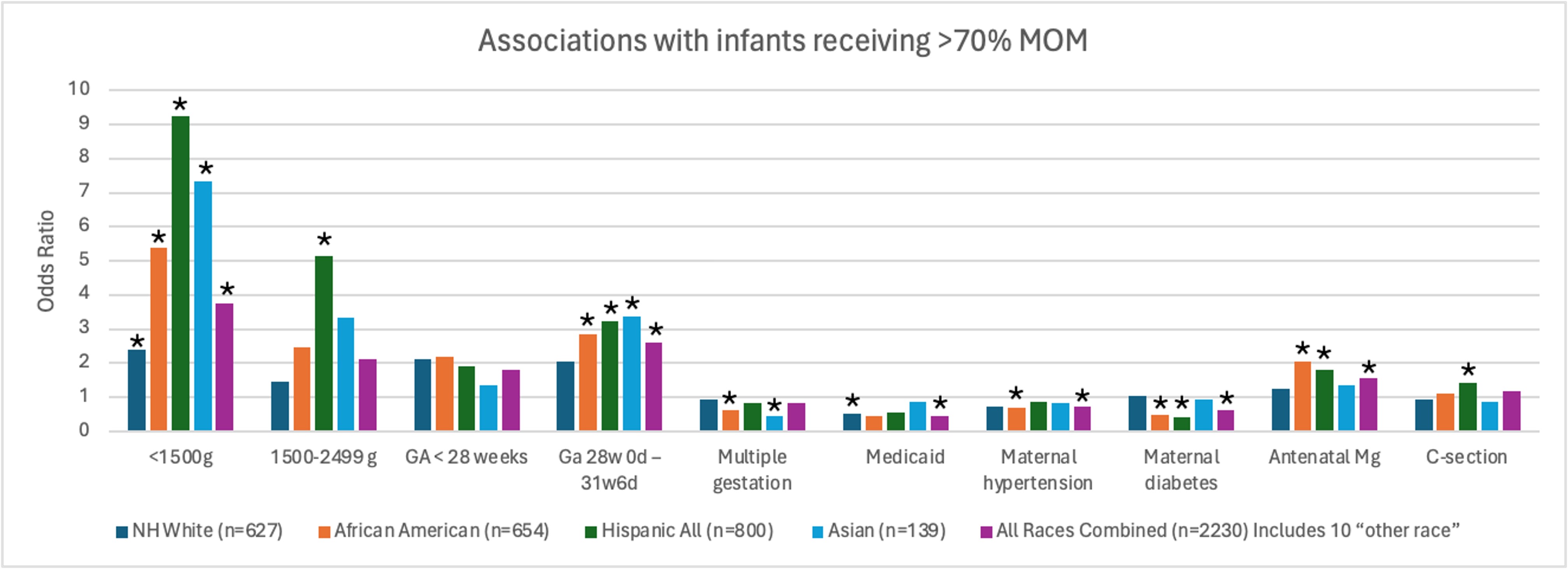 Odds of preterm infants receiving >70% MOM by Race and Ethnicity
Odds of preterm infants receiving >70% MOM by Race and EthnicityFigure 2
.jpg) Odds of Preterm infants receiving <30% MOM by birthweight
Odds of Preterm infants receiving <30% MOM by birthweight
