Breastfeeding/Human Milk 3
Session: Breastfeeding/Human Milk 3
668 - Quantifying the association between hypertensive disorders of pregnancy and breastfeeding non-initiation and cessation using CDC Pregnancy Risk Assessment Monitoring System
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 668.6142
Deanna Nardella, Yale School of Medicine, New Haven, CT, United States; Maureen Canavan, Yale University - - New Haven, CT, New Haven, CT, United States; Mona Sharifi, Yale School of Medicine, New Haven, CT, United States; Sarah Taylor, Yale School of Medicine, New Haven, CT, United States
- DN
Deanna Nardella, MD MHS (she/her/hers)
Instructor of Pediatrics
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Hypertensive disorders are drivers of US maternal and infant morbidity and mortality. Breastfeeding (BF) lowers maternal cardiometabolic risk, including hypertension risk. Yet, little is known about the relationship between maternal hypertensive disorders in the pre-pregnancy or pregnancy period(s) and BF outcomes.
Objective: To quantify if and to what extent maternal hypertensive disorders of pregnancy (HDP) are associated with never BF and postpartum BF cessation among a diverse, nationally representative sample of US women.
Design/Methods: We conducted a cross-sectional study using 2016-2022 data from the CDC Pregnancy Risk Assessment Monitoring System. Participants from 44 US states, DC and Puerto Rico were recruited between 2 to 4 months postpartum to complete a survey on pre-pregnancy, pregnancy, and postpartum experiences. Our sample included those who had a live infant and complete data for our exposure of a hypertensive disorder in the pre-pregnancy or pregnancy period(s), our outcomes of BF non-initiation or cessation, and our covariates, including sociodemographic, maternal health, and infant factors. HDP was defined as self-reported hypertension, pre-eclampsia, or eclampsia before or during pregnancy. We assessed differences in HDP prevalence by covariates using chi square tests. Adjusting for all covariates, we used multivariable logistic regression to assess the association between maternal HDP status and never BF (reporting adjusted odds ratios and predicted probabilities) and multivariable cox regression to quantify the hazard of postpartum BF cessation by maternal HDP.
Results: Our study cohort included 205,247 women (weighted N= 10,915,302), narrowed to 180,660 women (weighted N= 9,570,975) when examining only women who breastfed for our multivariable cox regression. Maternal HDP was more prevalent among individuals over 35 years of age, enrolled in Medicaid, with lower income and educational status, of non-Hispanic Black or American and Alaskan Native race or ethnicity, and who had prior children, multiple gestation, premature delivery, BMI > 30 kg/m2, diabetes, depression, or cesarean delivery (P < 0.001, Table 1). Maternal HDP was associated with 11% higher odds of never BF (aOR 1.11, 1.05-1.18, P< 0.001) and a 17% higher hazard of BF cessation in the postpartum period (aHR 1.17; 1.14-1.21, P< 0.001) (Table 2, Fig 1) compared with women who did not report HDP.
Conclusion(s): Maternal HDP was associated with higher odds of never BF and higher hazard of postpartum BF cessation within our national US sample. Tailored BF support may improve outcomes for dyads with higher cardiometabolic risk.
Table 1
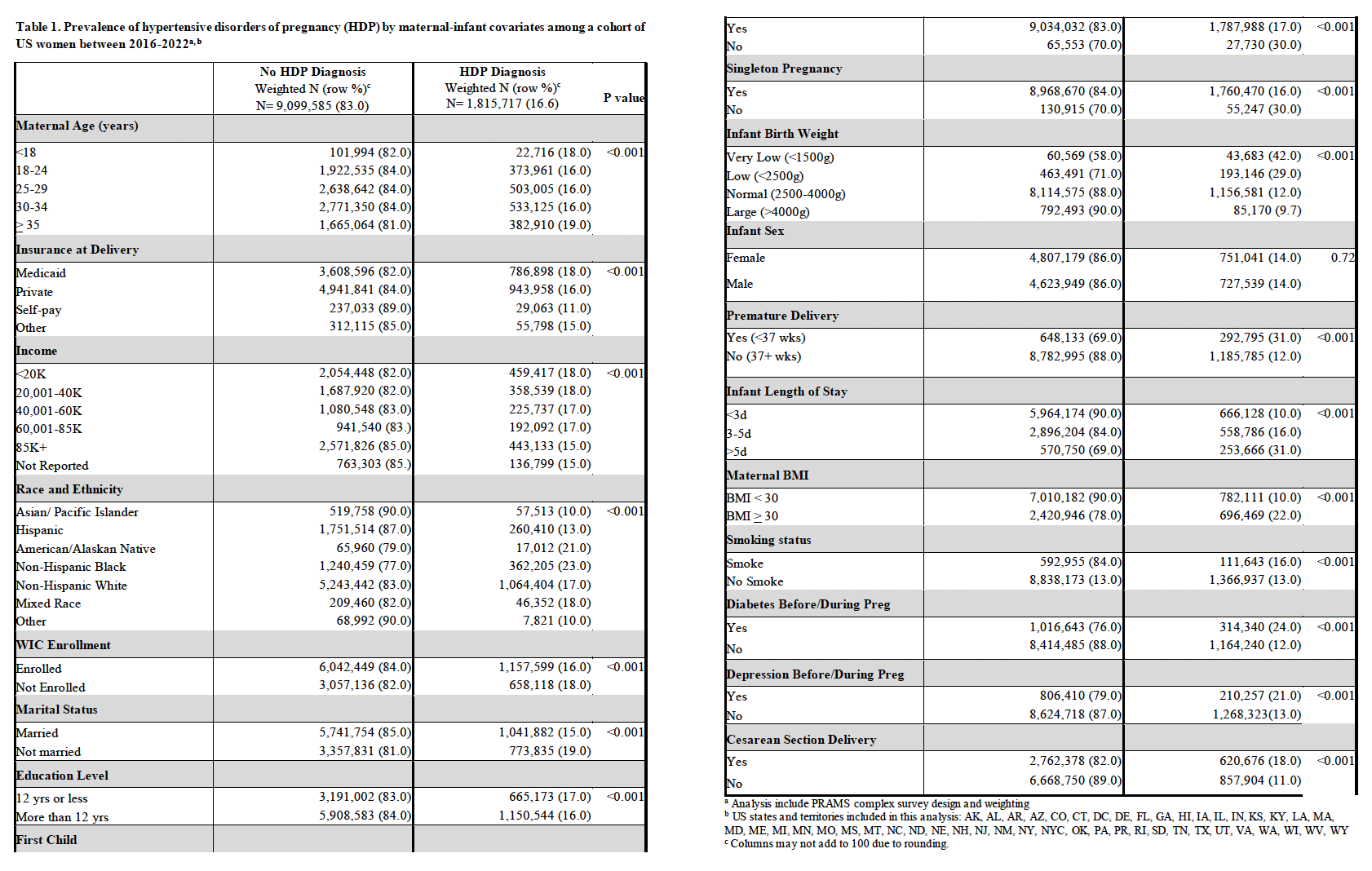 Prevalence of hypertensive disorders of pregnancy by maternal-infant covariates among a cohort of US women between 2016-2022
Prevalence of hypertensive disorders of pregnancy by maternal-infant covariates among a cohort of US women between 2016-2022Table 2
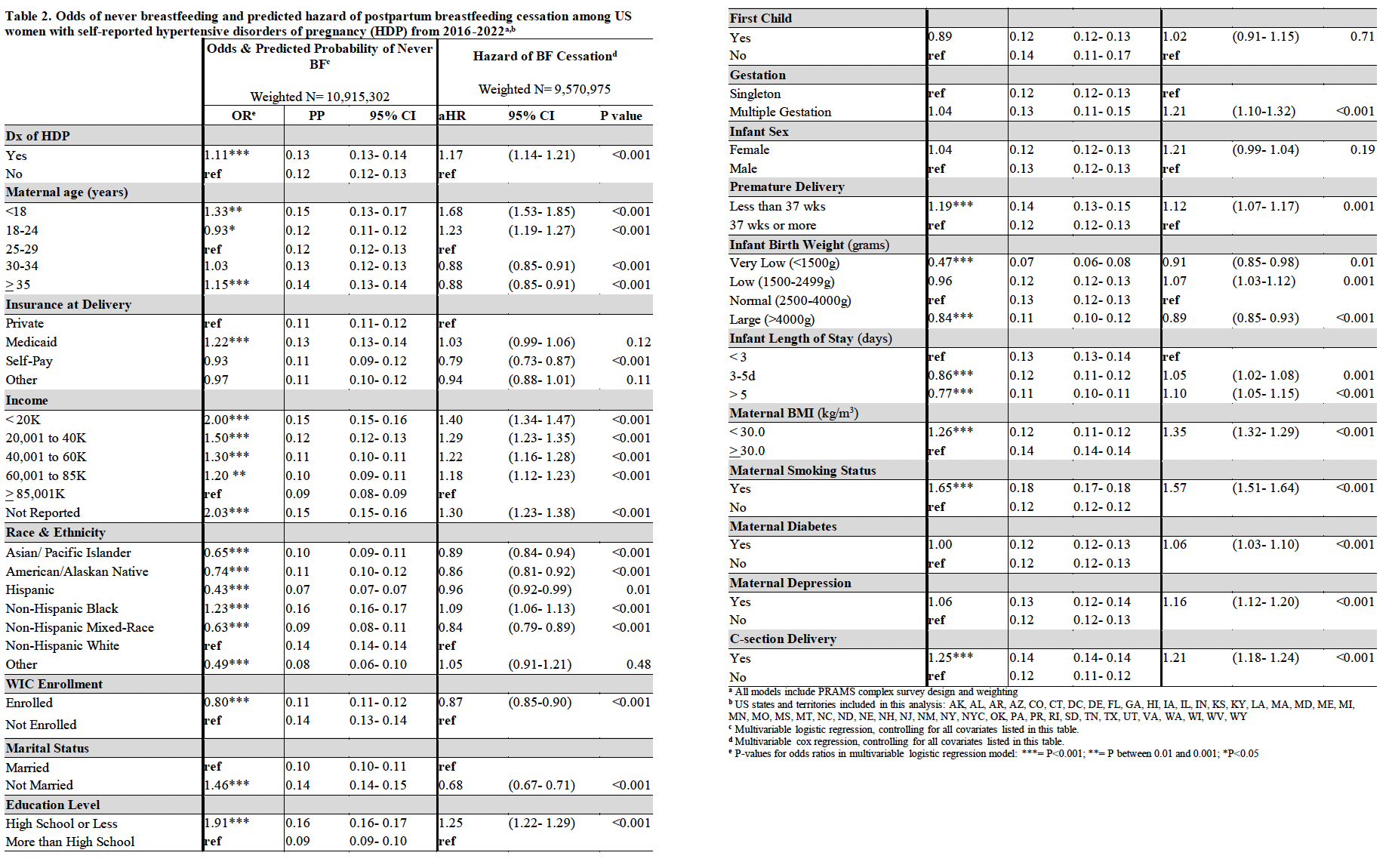 Odds of never breastfeeding and predicted hazard of postpartum breastfeeding cessation among US women with self-reported hypertensive disorders of pregnancy (HDP) from 2016-2022
Odds of never breastfeeding and predicted hazard of postpartum breastfeeding cessation among US women with self-reported hypertensive disorders of pregnancy (HDP) from 2016-2022Figure
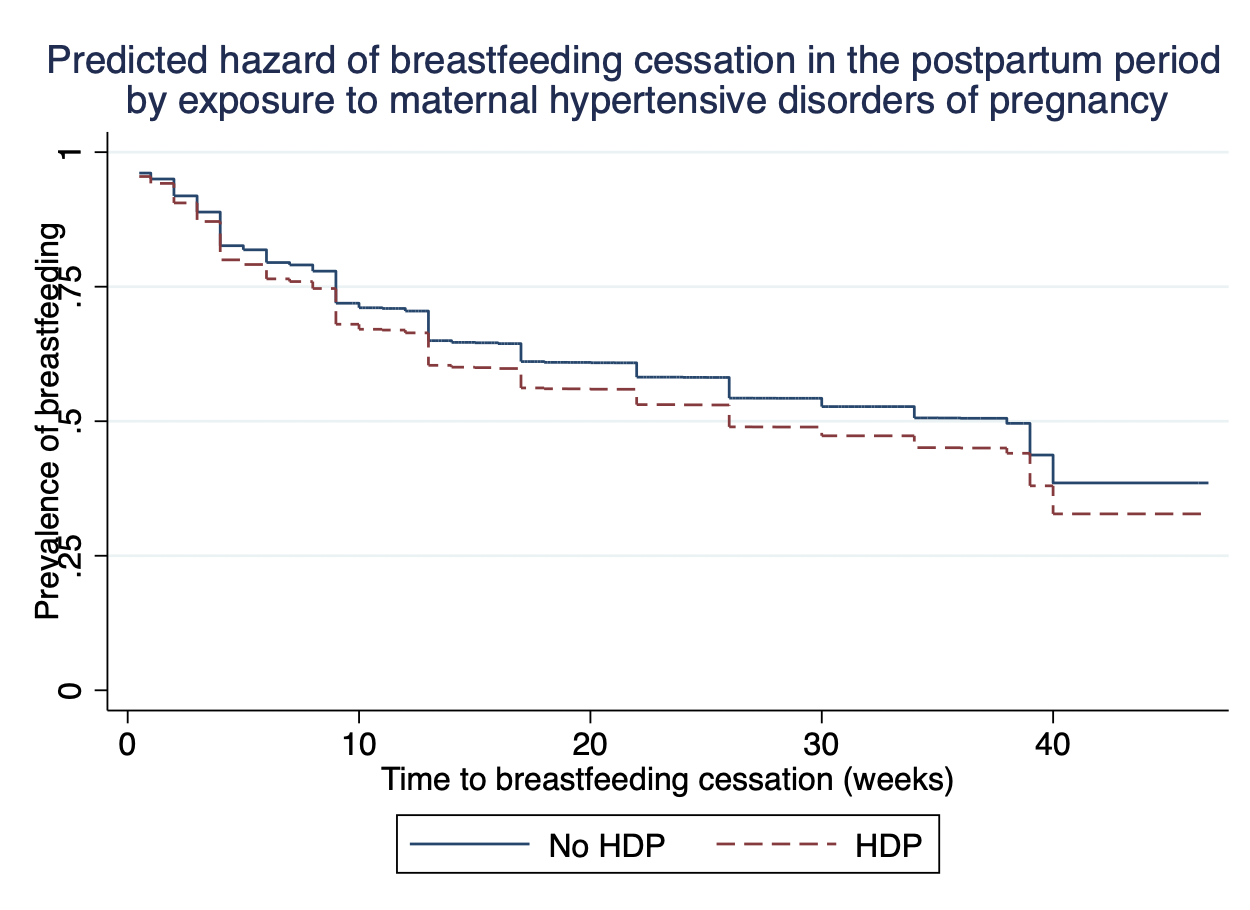 Predicted hazard of breastfeeding cessation in the postpartum period by exposure to maternal hypertensive disorders of pregnancy
Predicted hazard of breastfeeding cessation in the postpartum period by exposure to maternal hypertensive disorders of pregnancyTable 1
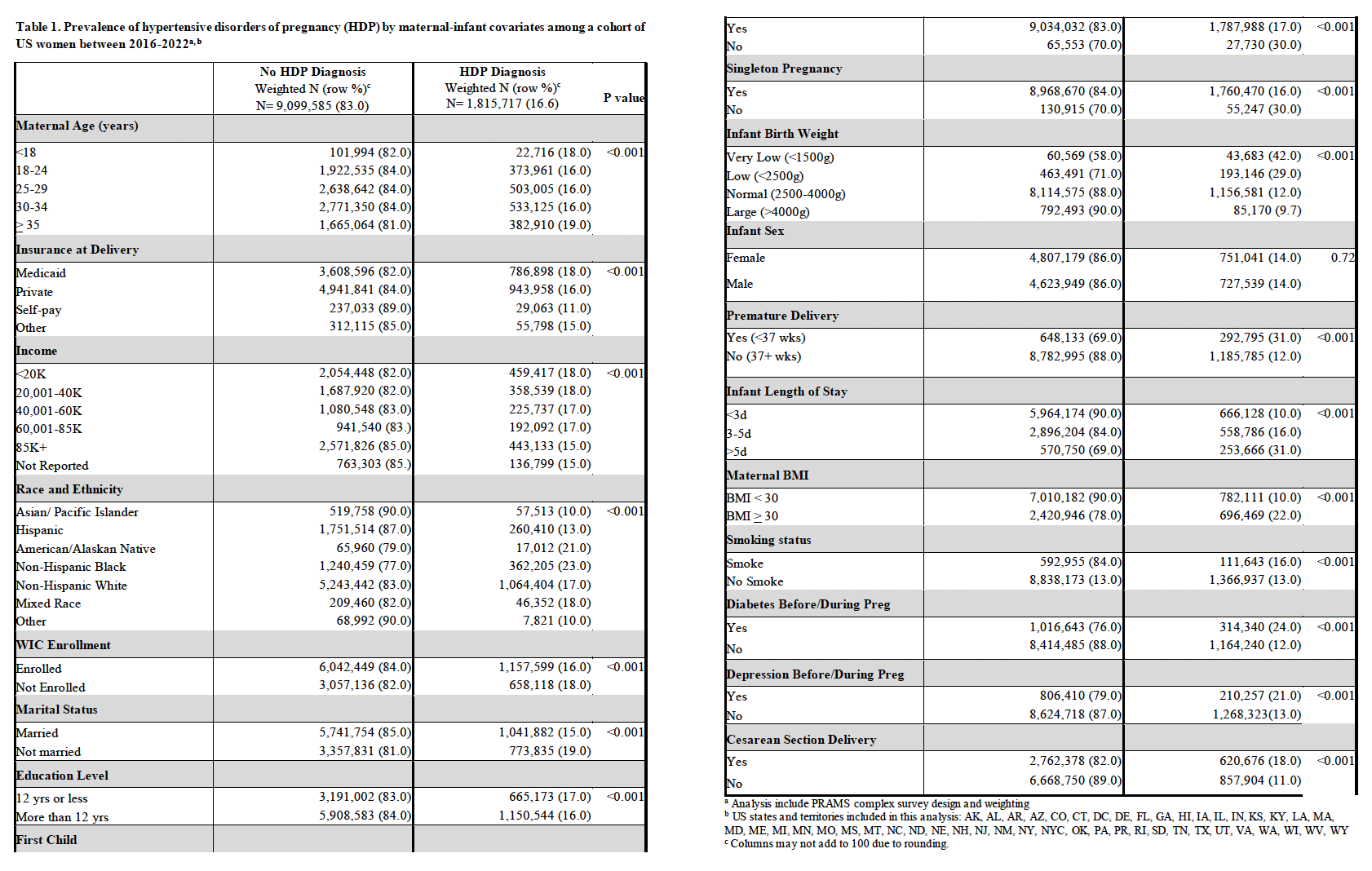 Prevalence of hypertensive disorders of pregnancy by maternal-infant covariates among a cohort of US women between 2016-2022
Prevalence of hypertensive disorders of pregnancy by maternal-infant covariates among a cohort of US women between 2016-2022Table 2
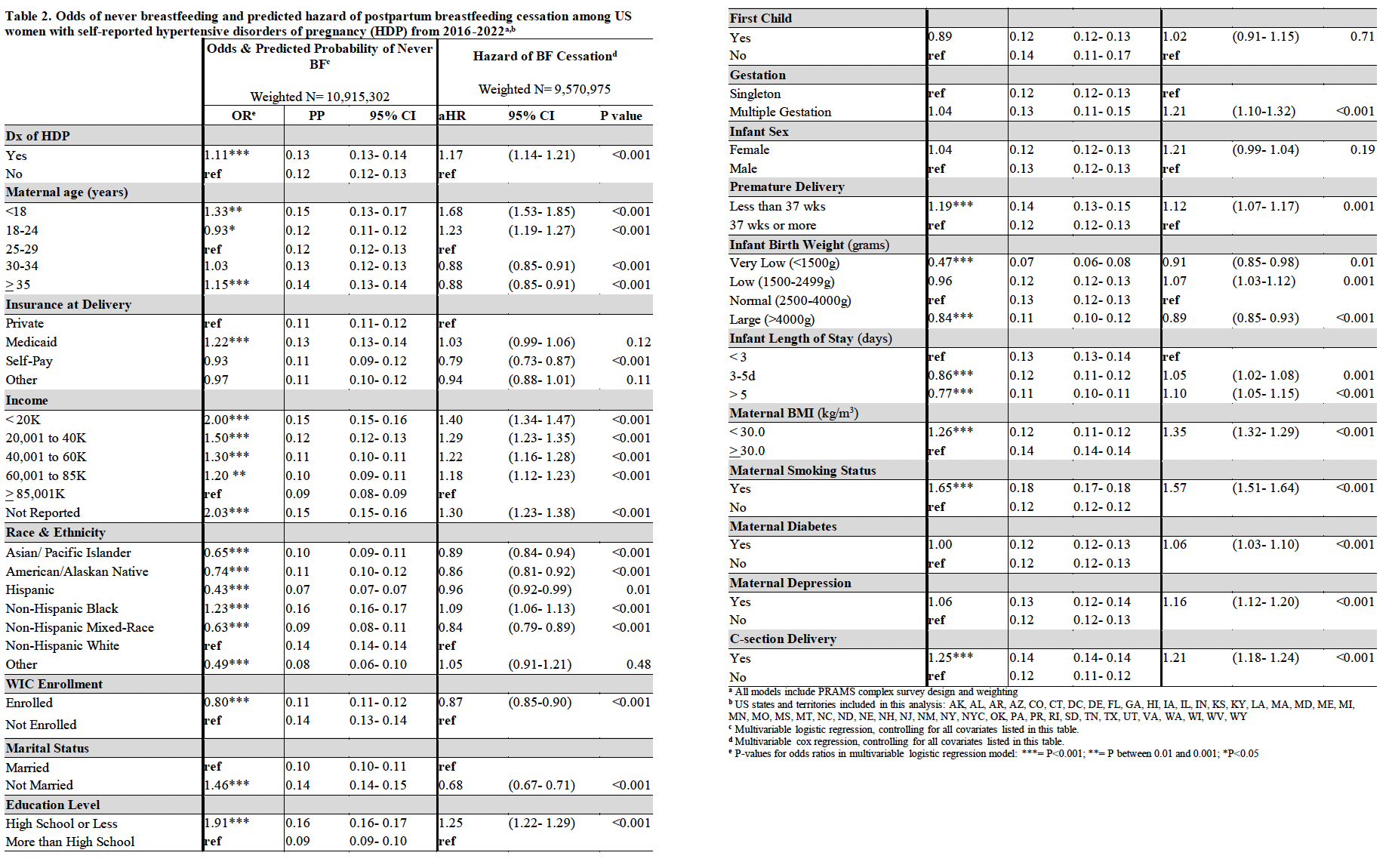 Odds of never breastfeeding and predicted hazard of postpartum breastfeeding cessation among US women with self-reported hypertensive disorders of pregnancy (HDP) from 2016-2022
Odds of never breastfeeding and predicted hazard of postpartum breastfeeding cessation among US women with self-reported hypertensive disorders of pregnancy (HDP) from 2016-2022Figure
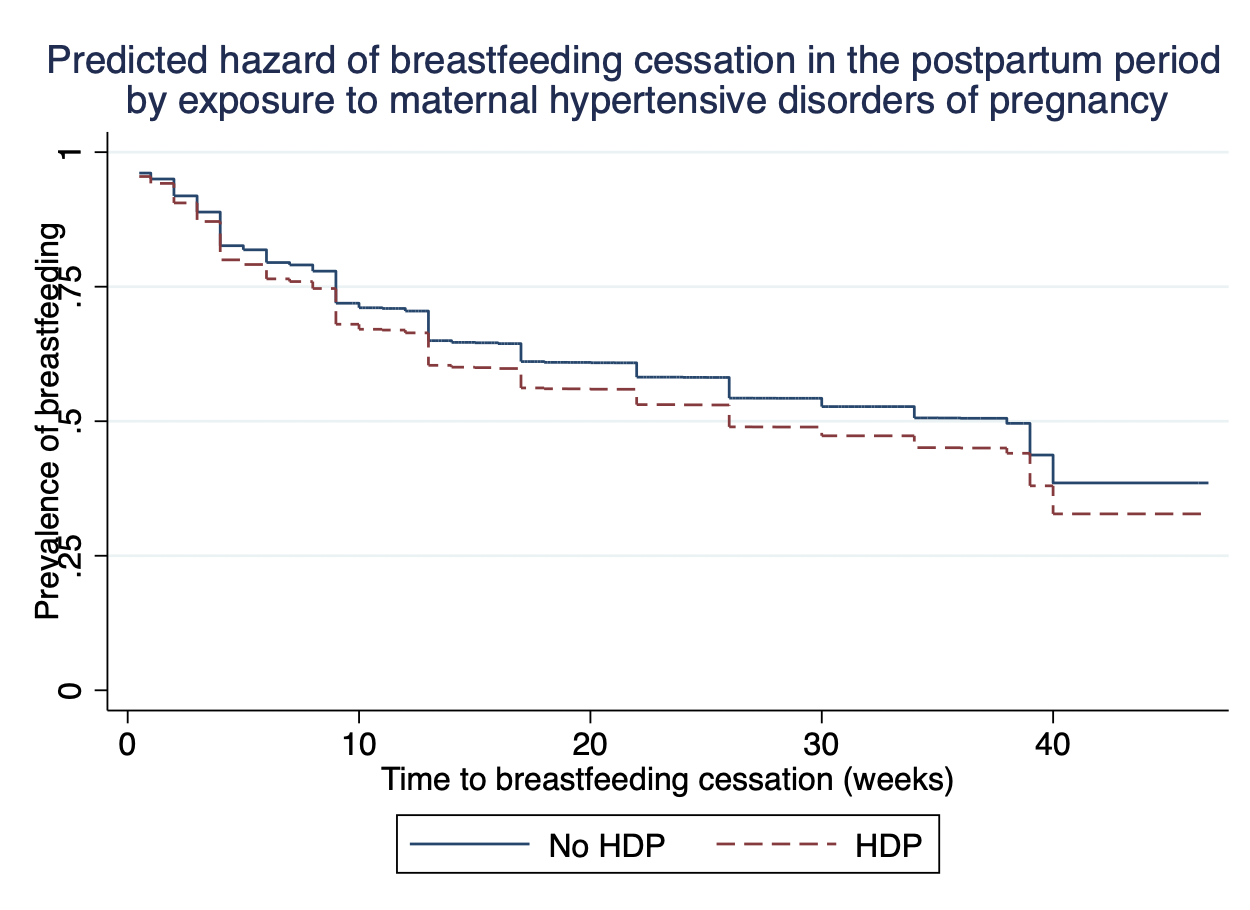 Predicted hazard of breastfeeding cessation in the postpartum period by exposure to maternal hypertensive disorders of pregnancy
Predicted hazard of breastfeeding cessation in the postpartum period by exposure to maternal hypertensive disorders of pregnancy
