Breastfeeding/Human Milk 2
Session: Breastfeeding/Human Milk 2
650 - Caregiver and Health Care Workers Perceptions about High Volume Breast Feeding in Low Birth Weight Preterm Infants in Zambia.
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 650.4152
Angelina A. Toluhi, University of Alabama at Birmingham (UAB), Birmingham, AL, United States; Lekan Ajijola, University of Alabama School of Medicine, Birmingham, AL, United States; Albert Manasyan, University of Alabama School of Medicine, Birmingham, AL, United States; Jyoti Lakhwani, Centre for Infectious Disease Research in Zambia, Lusaka, Lusaka, Zambia; Colm P. Travers, UAB, Birmingham, AL, United States; Rachel Sinkey, University of Alabama at Birmingham, Birmingham, AL, United States; Waldemar Carlo, UAB School of Medicine, Birmingham, AL, United States

Jyoti Lakhwani, MD, PGD Neonatology, MPH/MHLM (she/her/hers)
Fellow
Centre for Infectious Disease Research in Zambia
Lusaka, Lusaka, Zambia
Presenting Author(s)
Background: Preterm infants are at higher risk for postnatal growth restriction, leading to adverse short- and long-term developmental outcomes. Compared with usual volume (UV) feeding, higher volume (HV) (≥180 mL/kg/day) feeding increases growth velocity, postnatal growth, and weight at discharge among preterm infants.
Objective: We explored the acceptability, feasibility, and perception of feeding tolerance of HV feeding with breastmilk among mothers of preterm infants and healthcare workers (HCWs) in Lusaka, Zambia.
Design/Methods: Twenty-two (24) in-depth interviews (IDIs) were conducted with HCWs, including doctors, nurses, and dieticians (n=12) and mothers (n = 12) of low birthweight preterm infants admitted to the Kangaroo Mother Care (KMC) Ward at the University Teaching Hospital (UTH). Eligible mother-infant dyads were those whose infants were randomized to the HV study group (200-240 ml/kg/day) of the parent study as compared to the UV (140-180 ml/kg/day). Interviews were conducted in English, Nyanja, and Bemba. The audio recordings were transcribed and translated by trained research assistants and stored in a secure drive. Coding and analysis of transcripts were conducted using NVivo software (v14). A thematic analysis approach was used to identify emerging themes.
Results: Initial concerns expressed by mothers and HCWs about HV feeding for preterm infants included fear of aspiration, volume and feeding frequency, longer hospital stay, and ability to continue the same routine at home. Both mothers and HCWs observed that most newborns tolerated the HV feeding well. Some mothers experienced initial challenges with low milk volume production; however, with support and education, HCWs reported that mothers gained confidence and could independently express HV milk within 2-7 days of HV feeding. HCWs perceived that HV feeding led to faster weight gain, increased KMC predischarge readiness score, and fewer readmissions for babies without comorbidities. Mothers found HV feeding to be acceptable, were able to continue HV feeding post-discharge, and observed that their babies became more active and increased their weight and height rapidly.
Conclusion(s): HV breastfeeding was perceived as a feasible and acceptable way of improving weight and height gain, increasing KMC predischarge readiness scores and reducing readmissions in preterm newborns by both HCWs and mothers, particularly when integrated with KMC. Some HCWs suggested expanding the practice to include all preterm infants to optimize nutrition and weight gain in this population.
Illustrative Quotes
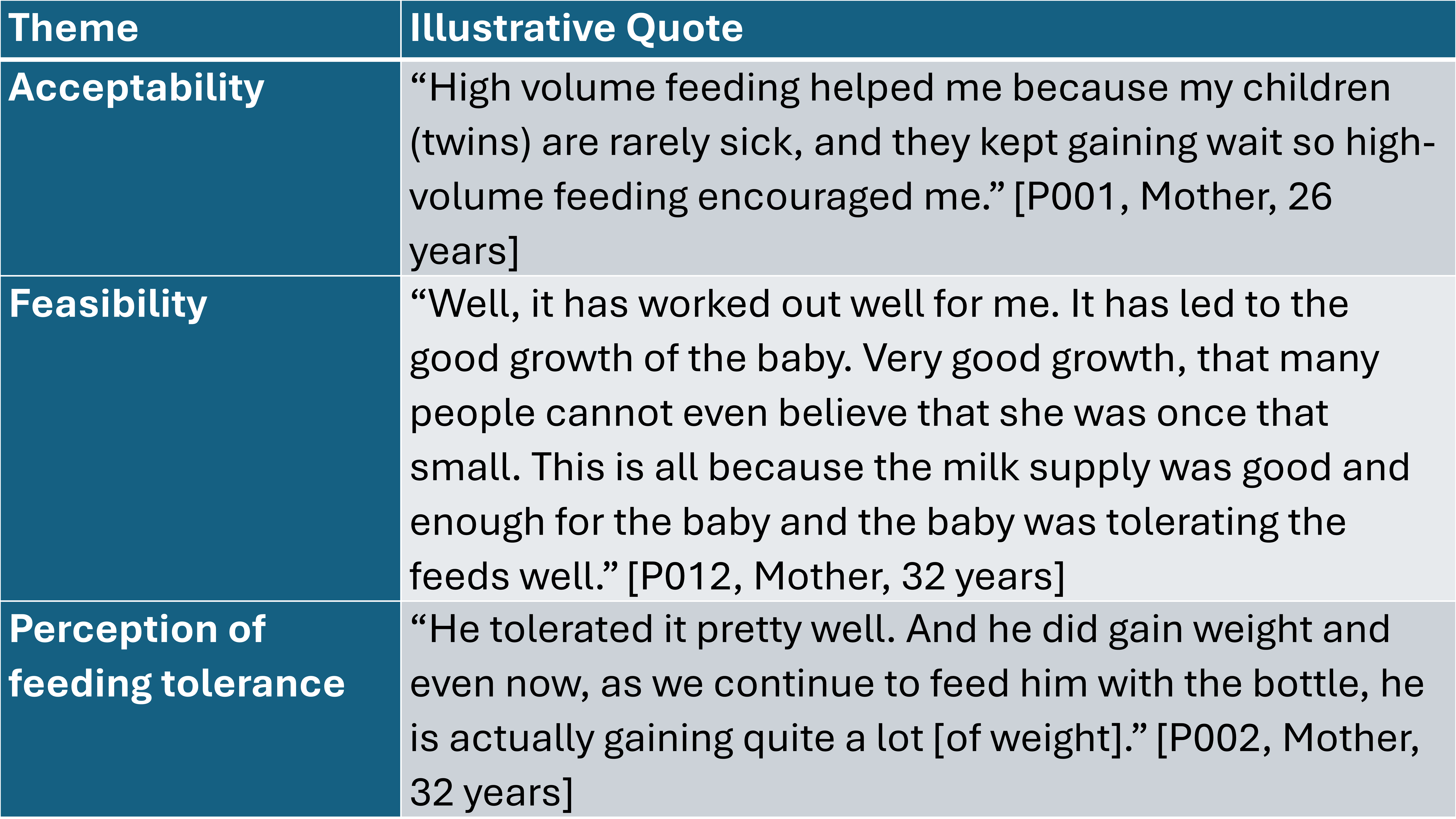 Illustrative quotes highlighting the acceptability, feasibility, and perceptions of feeding tolerance themes.
Illustrative quotes highlighting the acceptability, feasibility, and perceptions of feeding tolerance themes.
