Breastfeeding/Human Milk 3
Session: Breastfeeding/Human Milk 3
666 - Socioeconomic Disparities in Human Milk Nutrition Patterns Among Preterm Infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 666.6817
Igbagbosanmi Oredein, Stanford University School of Medicine, Palo Alto, CA, United States; Molly Lazarus, Stanford University School of Medicine, New York, NY, United States; Rachel Land, Stanford University School of Medicine, Sunnyvale, CA, United States; Katherine Travis, Weill Cornell Medicine, White Plains, NY, United States; Sonia L. Bonifacio, Stanford University School of Medicine, Los Altos, CA, United States; Melissa Scala, Stanford University School of Medicine, Palo Alto, CA, United States
.jpg)
Igbagbosanmi Oredein, MD, MPH
Neonatal-Perinatal Medicine Fellow
Stanford University School of Medicine
Menlo Park, California, United States
Presenting Author(s)
Background: Human milk (HM) is the recommended nutrition for preterm (PT) infants; however, disparities exist in its use. Although donor human milk (DHM) is thought to be the ideal alternative when mother’s own milk (MOM) is unavailable, several nutrients may be lacking in DHM, affecting growth and development. The trends of HM intake in the neonatal intensive care unit (NICU) when DHM is used are unknown.
Objective: This study aims to explore HM nutrition patterns among PT infants and investigate disparities therein.
Design/Methods: Retrospective cohort study of 124 PT infants in a single center level IV NICU. Infants born < 32 weeks gestational age (GA) in 2022 were included and those who died or received no HM before 34 weeks post menstrual age (PMA) were excluded. Data were obtained from the hospital HM tracking system, Timeless Medical Systems. Daily volume of HM intake was categorized into MOM and DHM. Total DHM percentage was calculated as total volume of DHM over total HM feeds till 34 weeks PMA. Insurance type was used as a surrogate marker for socioeconomic status (SES) with public insurance defined as low SES and private insurance as high SES.
Results: Across their hospitalization, infants from low SES groups received higher percentages of DHM than their high SES peers (42% vs. 24%, p < 0.001) and this difference remained when controlling for GA. There were also significant differences in ethnicity in the use of DHM (41% Hispanic vs 25% non-Hispanic infants; p = 0.002) however when controlled for SES, the disparity was not significant. Linear mixed modeling revealed that throughout the first 14 days of life (DOL), infants from high SES groups had a quicker drop in the percentage of DHM received (p < 0.001) indicating that they had a faster transition from receiving DHM to MOM. 48% of low SES infants were discharged home solely on formula feeds compared to 20% of high SES infants (p = 0.004). Logistic regression analysis controlling for GA revealed that DHM percentage on DOL 14 predicted home discharge on formula feeds (p < 0.001). There were no significant racial or language disparities related to DHM vs. MOM intake.
Conclusion(s): Socioeconomic disparities exist in nutrition patterns among PT infants. Infants from high SES groups receive higher volumes of MOM vs. DHM, transition from receiving DHM to MOM quicker and are less likely to be discharged on formula feeds when compared to infants from low SES groups. The amount of DHM feeds on DOL 14 may predict nutrition at discharge. Thus, the first 14 DOL may represent a unique opportunity to intervene and influence the outcome of HM feeding at discharge.
Figure 1.
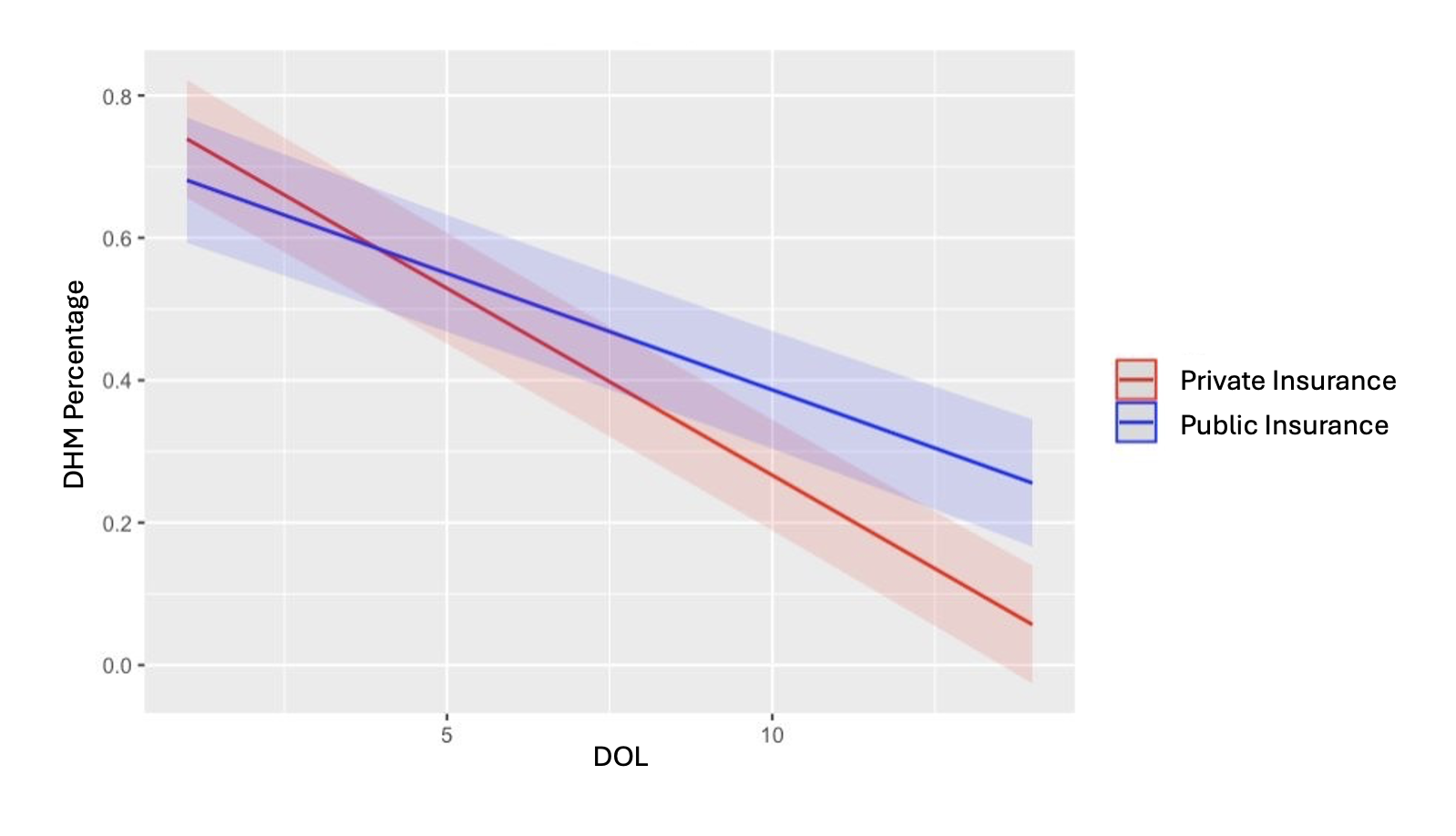 Modeled estimate of the interaction between Day of Life (DOL) and public insurance predicting Donor Human Milk (DHM) percentage while controlling for gestational age (GA)
Modeled estimate of the interaction between Day of Life (DOL) and public insurance predicting Donor Human Milk (DHM) percentage while controlling for gestational age (GA) Table 1.
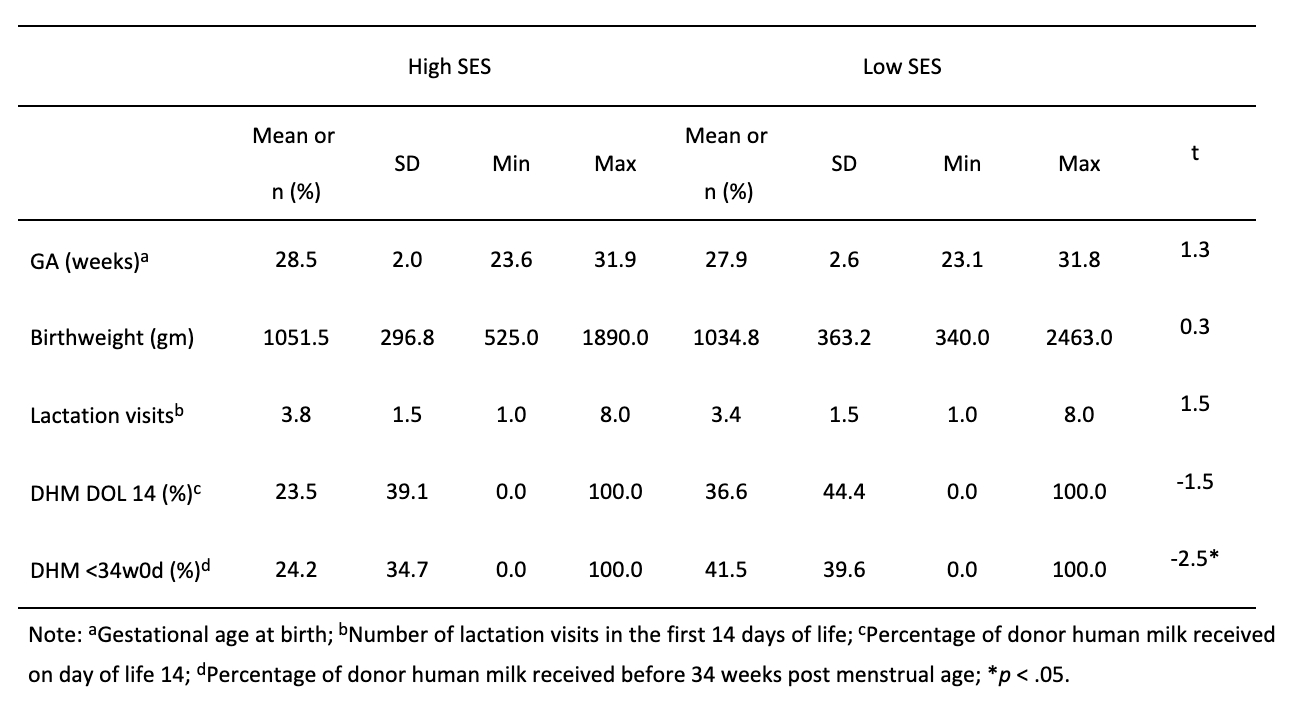 Comparison of clinical and demographic characteristics of infants in high- (n=67) vs. low-SES (n = 60) groups
Comparison of clinical and demographic characteristics of infants in high- (n=67) vs. low-SES (n = 60) groups 
