Breastfeeding/Human Milk 2
Session: Breastfeeding/Human Milk 2
649 - Timing and Intensity of Lactation Support Within the First Days of NICU Life Influences Discharge on Maternal Milk
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 649.6839
Chloe Salzmann, Medical, Milwaukee, WI, United States; Evan Cross, Medical College of Wisconsin, Milwaukee, WI, United States; Ke Yan, Medical College of Wisconsin, Milwaukee, WI, United States; Jian Zhang, Medical College of Wisconsin, Milwaukee, WI, United States; Erwin T. Cabacungan, Medical College of Wisconsin, Milwaukee, WI, United States; T. Hang Nghiem-Rao, Medical College of Wisconsin, Mil, WI, United States; Alicia Sprecher, Medical College of Wisconsin, Milwaukee, WI, United States

Chloe Salzmann, MD, IBCLC (she/her/hers)
Neonatology Fellow
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Maternal breast milk can be a life-saving intervention for infants cared for in the NICU; however, provision remains suboptimal. A better understanding of factors that influence sustained lactation are needed to guide interventions to improve the number of infants receiving maternal milk.
Objective: Our goal was to identify maternal and infant characteristics associated with infant discharge home on maternal milk and to evaluate the influence of early lactation support on sustaining lactation through NICU discharge.
Design/Methods: We conducted a retrospective chart review of inborn mother-infant dyads admitted to a level IV NICU between 1/1/2018 and 6/30/2023 with length of stay 14-120 days. Dyads were excluded if the infant died before NICU discharge, or if the mother was absent, was < 18 years old, or had a contraindication to lactation. Maternal data included demographics, socioeconomic factors, medical history, and obstetric factors. Infant data included demographics, aspects of clinical care, and diagnoses. Our outcome of interest was discharge receiving any maternal milk. Logistic regression was utilized to predict discharge on maternal milk and generate odd ratios and p-values.
Results: We analyzed data for 862 maternal infant dyads (Fig 1). Infants discharged on formula were more often born to Black, multiparous mothers with public insurance, lower household income, lower intent to breastfeed, and were more likely delivered via c-section, at a lower gestational age, and with lower birth weight. (Tables 1A&B). Days to lactation consultation and frequency of lactation consultation within the first 2 weeks were both significantly associated with discharge on maternal milk (Table 2). Infants were significantly less likely to discharge home receiving maternal milk if their mothers were seen by lactation on day 2 post-partum compared to days 0 or 1 (OR 0.56 [95% CI 0.33-0.94] and OR 0.46 [95% CI 0.28-0.75], P< 0.05 for both comparisons), Fig.2A. Infants whose mothers who had 4-6 lactation visits within the first 14 days were 6.29 times more likely discharge home receiving maternal milk than those whose mothers had less than 4 visits (95% CI 3.95-10.02, P< 0.05), Fig. 2B.
Conclusion(s): Lactation consultants play a key role in supporting parents in establishing milk supply. Lactation consultation within the first 48 hours post-partum and at least 4 lactation visits within the first 2 weeks post-partum improves the number of infants discharged from the NICU on maternal milk. Staffing considerations in hospitals with access to lactation consultants should account for this need.
Figure 1
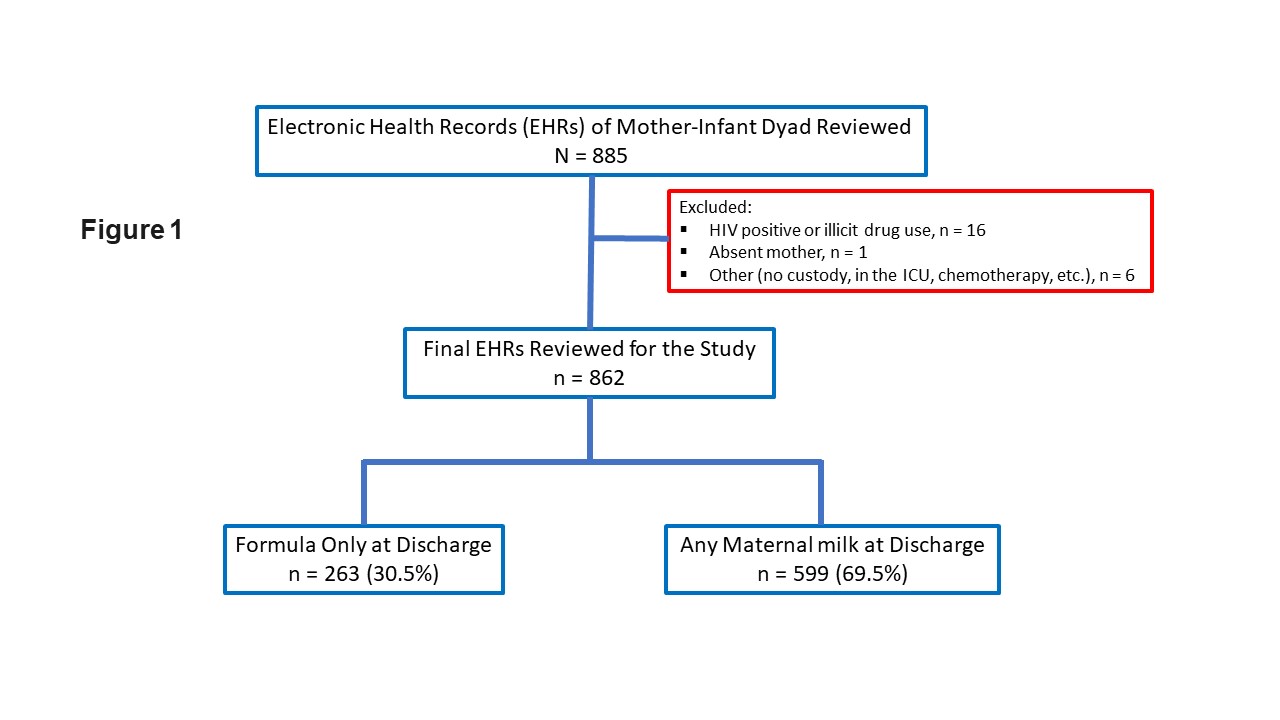 Mother/Infant dyads reviewed and number discharged on any maternal milk.
Mother/Infant dyads reviewed and number discharged on any maternal milk.Tables 1A and 1B
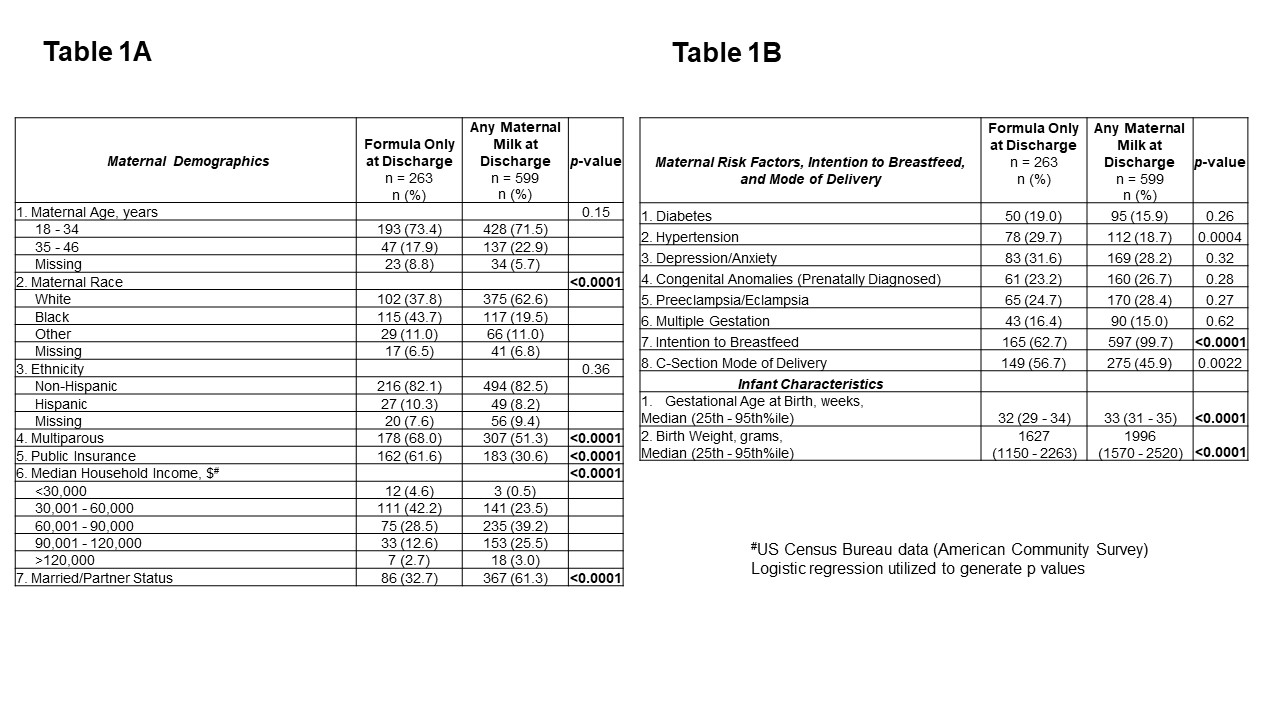 Maternal demographics and risk factors affecting discharge on mother's milk.
Maternal demographics and risk factors affecting discharge on mother's milk.Table 2 and Figures 2A and 2B
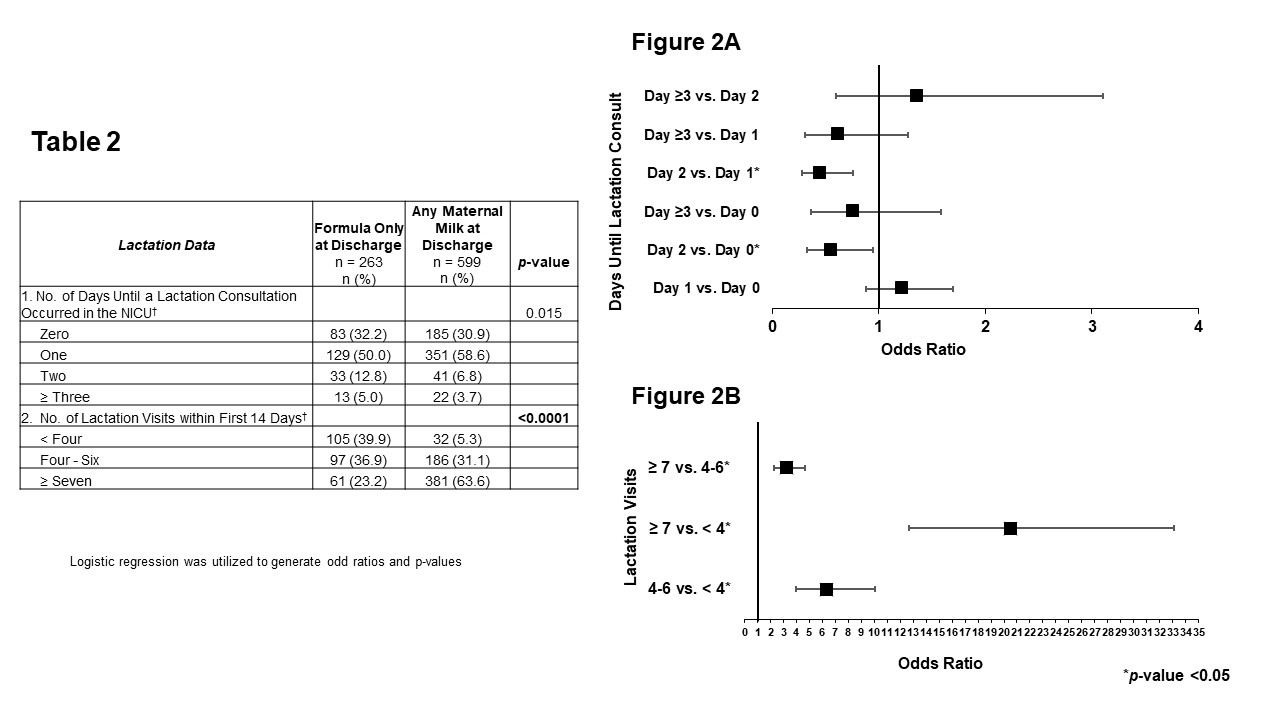 Days to lactation consultation and frequency of lactation consults within first two visits were associated with discharge on mother's milk.
Days to lactation consultation and frequency of lactation consults within first two visits were associated with discharge on mother's milk.
