Health Services Research 1: Workforce & Underserved Areas
Session: Health Services Research 1: Workforce & Underserved Areas
292 - Combined effects of rurality and race/ethnicity on pediatric tonsillectomy rates
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 292.4134
Colleen McLaughlin, Nationwide Children's Hospital, Columbus, OH, United States; Jesse L. Hawke, Nationwide Children's Hospital, Columbus, OH, United States; Emily F. Boss, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Meredith Lind, Nationwide Children's Hospital/ The Ohio State Universoty, Powell, OH, United States; Tasleem J. Padamsee, The Ohio State University College of Public Health, Columbus, OH, United States; Prasanth Pattisapu, Nationwide Children's Hospital, Columbus, OH, United States; Deena J. Chisolm, Nationwide Childrens Hospital, Columbus, OH, United States; Laura Chavez, Nationwide Children's Hospital, Columbus, OH, United States; Guy Brock, The Ohio State University, Columbus, OH, United States

Colleen McLaughlin, MPH PhD (she/her/hers)
Research Scientist
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Tonsillectomy is one of the most common surgical procedures requiring general anesthesia performed on children in the US. Higher rates of tonsillectomy have been observed in rural relative to urban settings and among White non-Hispanic (NH) children relative to Hispanic and Black NH children.
Objective: To determine whether associations between race/ethnicity and rates of pediatric tonsillectomy vary by urban/rural residence in the United States.
Design/Methods: Utilizing data from fifteen States participating in US Medicaid and Child Health Insurance Programs, we identified children ages two to 18 years with an otolaryngology visit (1/1/2017-6/30/2019) for either throat infection (n=64,972) or obstructive sleep disordered breathing (oSDB) without throat infection (n=111,756), the most common indications for tonsillectomy. We compared rates of tonsillectomy use within 6 months after initial otolaryngology visit for Black NH, Hispanic, or White NH children by urban or rural classification of their ZIP Code of residence.
Results: The association of race and ethnicity with tonsillectomy rates was significantly modified by urban/rural residence (Table 1, Figure 1). After adjustment for age, sex, and clinical factors, tonsillectomy rates did not differ significantly between rural Black NH and White NH children (42.8% and 42.6%, p=0.8410) with oSDB, and both groups had higher tonsillectomy rates than rural Hispanic children (38.9%, p< 0.0001). However, urban White NH children with oSDB (41.3%) had higher rates of tonsillectomy than urban Black NH children (38.4%, p< 0.0001) and urban Hispanic children (36.1%, p< 0.0001). For throat infection, higher rates of tonsillectomy were observed among White NH children (31.9% rural; 31.0% urban), relative to both Black NH (rural 29.1%, p = 0.0015; urban 25.1%, p< 0.0001) and Hispanic (rural 27.2%, p< 0.0001; urban 25.7%, p< 0.0001) children. Tonsillectomy rates were higher in rural compared to urban settings across all racial/ethnic comparisons (p < 0.01 for all comparisons).
Conclusion(s): Differences in tonsillectomy rates among Black NH children relative to White NH children were more pronounced in urban settings. Hispanic children relative to White NH children had lower tonsillectomy rates in both urban and rural settings, and differences for oSDB were less pronounced in urban areas. Potentially unwarranted geographic and racial/ethnic variation in tonsillectomy use deserves closer scrutiny to ensure appropriate and equitable care for all children.
Table 1. Adjusted pediatric tonsillectomy rates and rate differences following otolaryngology visit for throat infection or obstructive sleep disordered breathing, by Race/Ethnicity and Rurality1
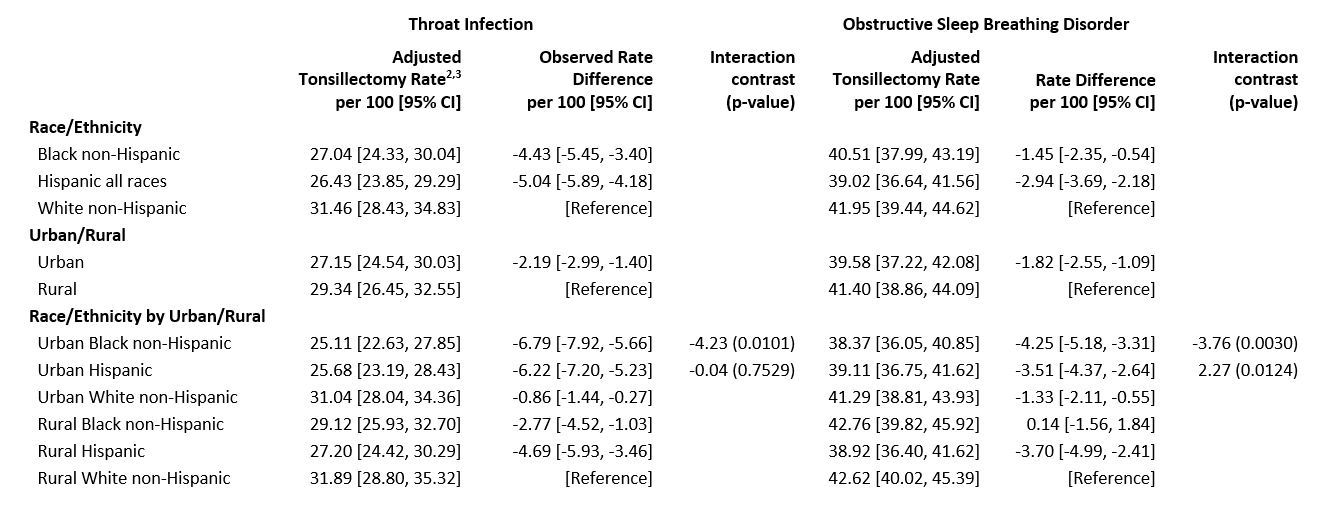 1. Medicaid/Child Health Insurance Program, United States, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, Washington
1. Medicaid/Child Health Insurance Program, United States, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, Washington 2. Rates are expressed as the percent of beneficiaries who had a tonsillectomy over 6 months of follow-up following index visit
3. Rates, rate differences, and interaction contrast adjusted for State, sex, age, race/ethnicity, urban/rural, obesity, asthma, throat infection, attention deficit/hyperactivity disorder, and polysomnography before and after otolaryngology visit
Abbreviations Used: CI=Confidence Interval
Figure 1. Interaction effects of race/ethnicity and rurality on adjusted pediatric tonsillectomy rates following otolaryngology visit, Medicaid/Child Health Insurance Program, United States, 2017- 2019
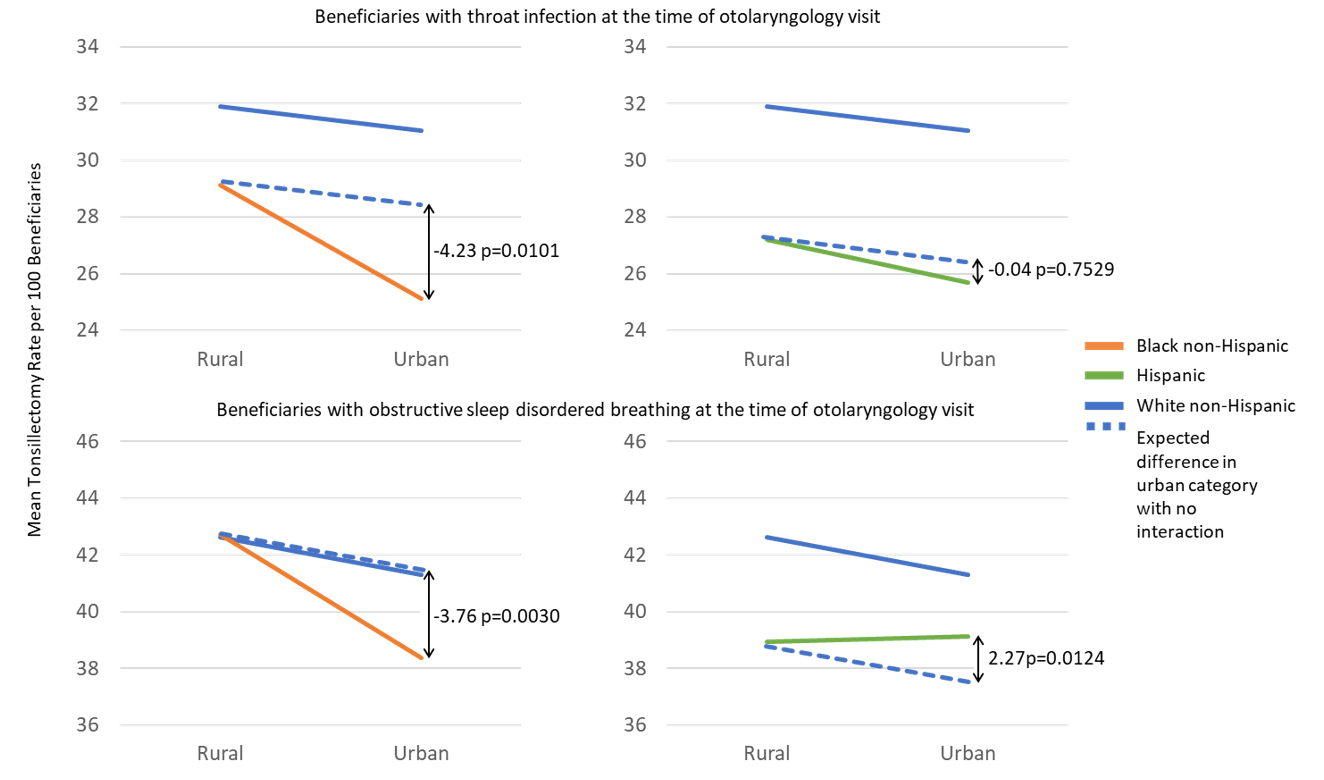 Medicaid/Child Health Insurance Program, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, and Washington. Rates are expressed as the percent of beneficiaries who had a tonsillectomy over 6 months of follow-up following otolaryngology visit, adjusted for State, sex, age, obesity, asthma, throat infection, attention deficit/hyperactivity disorder, and polysomnography before and after otolaryngology visit
Medicaid/Child Health Insurance Program, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, and Washington. Rates are expressed as the percent of beneficiaries who had a tonsillectomy over 6 months of follow-up following otolaryngology visit, adjusted for State, sex, age, obesity, asthma, throat infection, attention deficit/hyperactivity disorder, and polysomnography before and after otolaryngology visitTable 1. Adjusted pediatric tonsillectomy rates and rate differences following otolaryngology visit for throat infection or obstructive sleep disordered breathing, by Race/Ethnicity and Rurality1
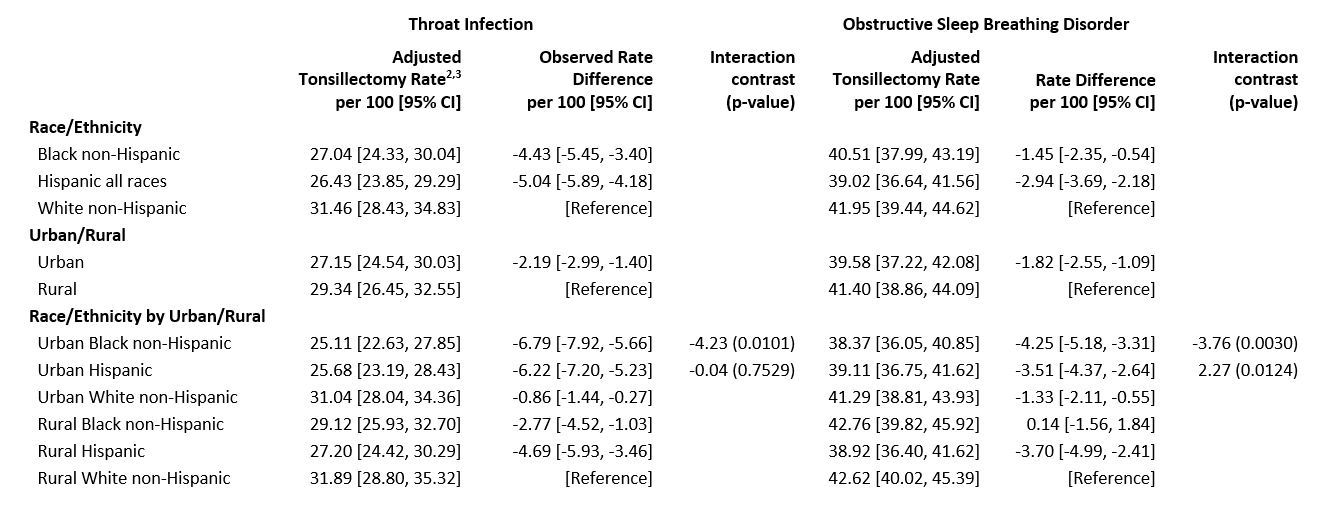 1. Medicaid/Child Health Insurance Program, United States, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, Washington
1. Medicaid/Child Health Insurance Program, United States, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, Washington 2. Rates are expressed as the percent of beneficiaries who had a tonsillectomy over 6 months of follow-up following index visit
3. Rates, rate differences, and interaction contrast adjusted for State, sex, age, race/ethnicity, urban/rural, obesity, asthma, throat infection, attention deficit/hyperactivity disorder, and polysomnography before and after otolaryngology visit
Abbreviations Used: CI=Confidence Interval
Figure 1. Interaction effects of race/ethnicity and rurality on adjusted pediatric tonsillectomy rates following otolaryngology visit, Medicaid/Child Health Insurance Program, United States, 2017- 2019
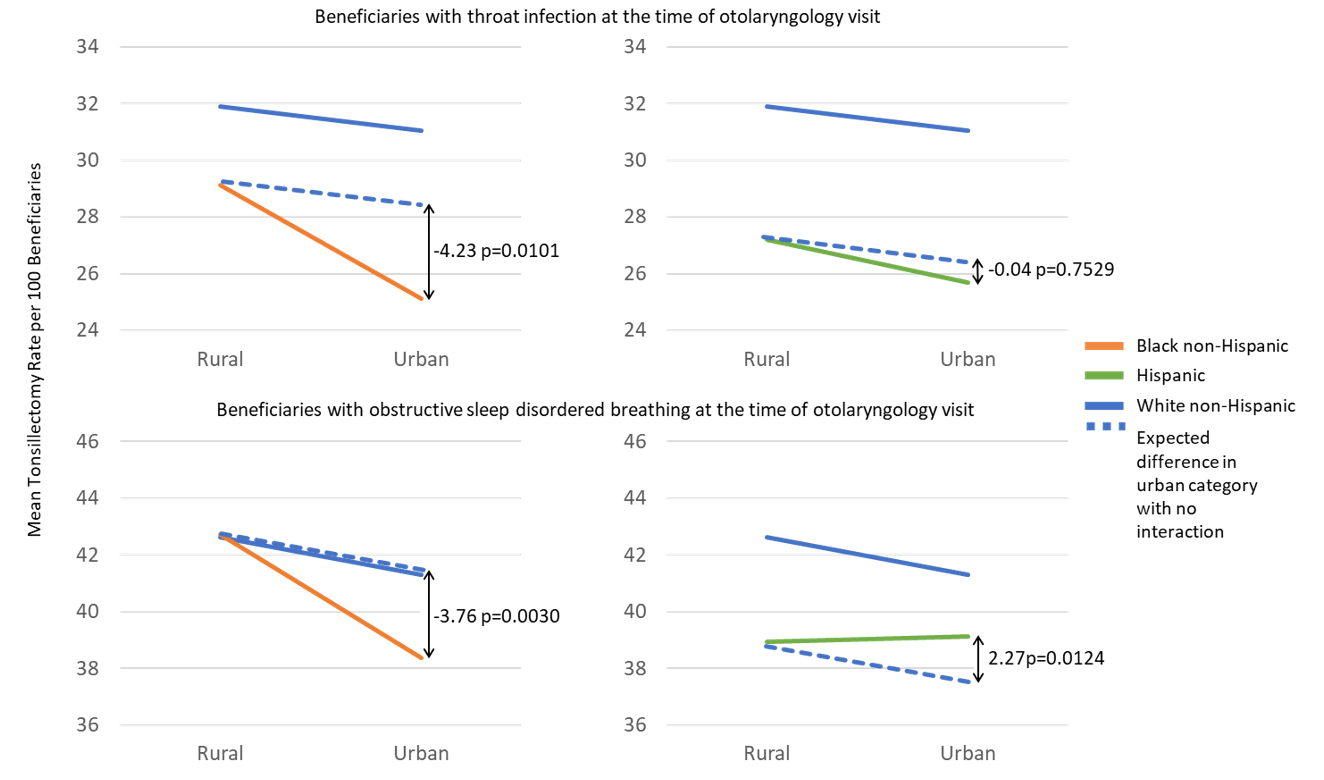 Medicaid/Child Health Insurance Program, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, and Washington. Rates are expressed as the percent of beneficiaries who had a tonsillectomy over 6 months of follow-up following otolaryngology visit, adjusted for State, sex, age, obesity, asthma, throat infection, attention deficit/hyperactivity disorder, and polysomnography before and after otolaryngology visit
Medicaid/Child Health Insurance Program, Jan 1, 2017-Jun 30, 2019, from California, Delaware, Florida, Indiana, Kentucky, Maine, North Carolina, New Hampshire, Nevada, Ohio, Oklahoma, Pennsylvania, South Dakota, Texas, and Washington. Rates are expressed as the percent of beneficiaries who had a tonsillectomy over 6 months of follow-up following otolaryngology visit, adjusted for State, sex, age, obesity, asthma, throat infection, attention deficit/hyperactivity disorder, and polysomnography before and after otolaryngology visit
