Breastfeeding/Human Milk 2
Session: Breastfeeding/Human Milk 2
662 - Temporal Dynamics of Hyaluronic Acid in Preterm Human Milk and its Associations with Gestational Age and Birth Weight
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 662.6653
Joan Lien, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Lise DeShea, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Jeffrey Eckert, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Addison Franca, University of Oklahoma Health Sciences Center, Oklahoma City, OK, United States; Kathryn Burge, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Hala Chaaban, Oklahoma University health sciences, Okl, OK, United States
Joan Lien, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Oklahoma College of Medicine
Oklahoma City, Oklahoma, United States
Presenting Author(s)
Background: Human milk (HM) is rich in bioactive components that support immune function, gut health, and growth. Concentrations of bioactive factors like hyaluronic acid (HA) vary among mothers and over time, potentially affecting infant susceptibility to conditions like necrotizing enterocolitis (NEC). HA is crucial for promoting intestinal health, mediating microbiome homeostasis, and reducing NEC risk in preclinical models. Data on HA concentrations in preterm HM is limited. Understanding HA levels in relation to maternal and infant characteristics may provide insights into factors influencing early protective benefits.
Objective: To characterize the temporal variation of HA in preterm HM over the first 10 weeks postpartum and to compare mothers with higher vs lower HA levels at 2 weeks postpartum.
Design/Methods: Infants born between 23 0/7 and 32 6/7 weeks’ gestational age (GA) and admitted to the Level IV NICU at Oklahoma Children’s Hospital were enrolled. Unfortified HM samples were collected weekly, frozen, and stored at -80°C. HA was quantified by ELISA. Demographics, feeding data, and growth measurements were recorded. Descriptive statistics and Wilcoxon signed-rank tests were used to compare HA concentrations over time (n>20 per time point). To look for associations between HA concentrations and other factors, the cohort was stratified into tertiles at 2 weeks postpartum based on HA concentrations.
Results: N=152 milk samples were collected from mothers of 34 preterm infants (Table 1). Colostrum had the highest median HA concentration (966.5 ng/mL, n=5). Figure 1 shows how HA levels varied widely among mothers during the first 3 weeks, declined, and stabilized at lower concentrations by week 4. Analysis between tertiles at week 2 showed no significant differences in maternal factors (Table 1). Compared to infants in the lower HA tertile (T1), those in the higher HA tertile (T3) had lower GAs (median 26 weeks vs 30 weeks) and lower birth weights (median 920g vs 1,465g), though these differences were not statistically significant (Table 2).
Conclusion(s): Variability of HA decreased over time, with the highest levels found in colostrum, though colostrum samples were limited. Unlike term milk’s gradual decline in HA over 2 months, preterm HM dropped earlier in the initial weeks of lactation, suggesting a potentially shorter window of protective effects. Future larger sample size of infants will investigate whether these differences reflect an increased need for HA-mediated gut protection in extremely low birth weight infants and will assess the impact of HA levels on growth trajectories and clinical outcomes.
Table 1.
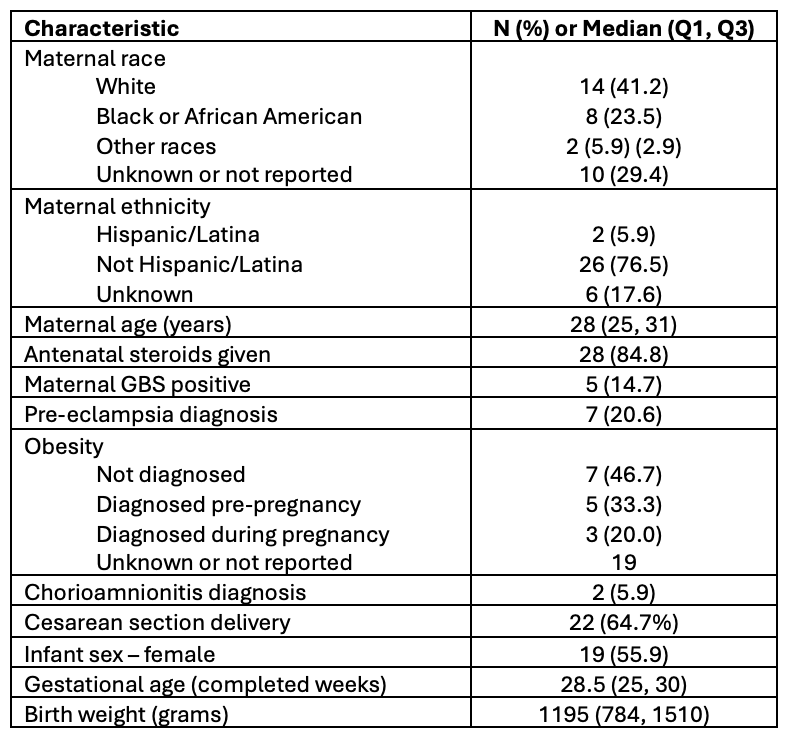 Maternal and infant demographics for the study population. Data are presented as N (%) for categorical variables or Median (Q1, Q3) for continuous variables.
Maternal and infant demographics for the study population. Data are presented as N (%) for categorical variables or Median (Q1, Q3) for continuous variables.Table 2.
.png) Descriptive statistics for groups based on HA concentration tertiles (T1 vs. T3) at measured Week 2. Data are presented as N (%) for categorical variables or Median (Q1, Q3) for continuous variables.
Descriptive statistics for groups based on HA concentration tertiles (T1 vs. T3) at measured Week 2. Data are presented as N (%) for categorical variables or Median (Q1, Q3) for continuous variables.Figure 1.
.png) Temporal changes in hyaluronic acid (HA) concentrations in preterm human milk over the first 10 weeks of lactation. Colostrum (Col., days 0-3 postpartum) shows the highest concentrations of HA, with marked variability among samples. HA levels decreased rapidly over the first few weeks of lactation and stabilized at lower concentrations after week 4.
Temporal changes in hyaluronic acid (HA) concentrations in preterm human milk over the first 10 weeks of lactation. Colostrum (Col., days 0-3 postpartum) shows the highest concentrations of HA, with marked variability among samples. HA levels decreased rapidly over the first few weeks of lactation and stabilized at lower concentrations after week 4.
