Neonatal GI Physiology & NEC 2
Session: Neonatal GI Physiology & NEC 2
733 - Association of fentanyl-induced microbiome changes and 2-year neurodevelopmental outcomes in preterm infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 733.3764
Pyone David, University of Chicago Comer Children's Hospital, Chicago, IL, United States; Kaitlyn Oliphant, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Christina Zhou, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Allen Wang, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Evanston, IL, United States; Bree Andrews, University of Chicago, Chicago, IL, United States; Erika C. Claud, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States
Pyone David, MD, MSW (she/her/hers)
Fellow
University of Chicago Comer Children's Hospital
Chicago, Illinois, United States
Presenting Author(s)
Background: Preterm infants are susceptible to poor growth and adverse clinical outcomes. Fentanyl, a commonly used medication for analgesia, has been implicated in gastrointestinal secretion and dysmotility. These changes may negatively influence gut microbiome development.
Objective: To assess the association of gut microbiome development and subsequent 2-year neurodevelopmental outcomes among preterm infants with postnatal fentanyl exposure.
Design/Methods: Microbiome In Neonatal Development (MIND), an IRB-approved study (IRB16-1431), recruited infants born < 37 weeks gestational age from the neonatal intensive care unit (NICU) at the University of Chicago Comer Children’s Hospital. A subset analysis of those surviving to discharge with stool samples from hospitalization and/or neurodevelopment outcomes (n = 68) compared those with (n = 46) and without (n = 22) fentanyl exposure. Analysis was adjusted for the delivery mode, sex, postmenstrual age, intrauterine and extrauterine growth differences, enteral feeds, antibiotics, and clinical morbidities. The α-diversity and relative abundances of individual bacterial taxa were assessed in fecal samples collected during hospitalization by 16S rRNA gene sequencing. Trimethylsilyl (TMS) Derivatization Protocol for Metabolite Profiling by Gas Chromatography-Mass Spectrometry (GC-MS) was performed on fecal samples collected during hospitalization. At 24 months of age, the Bayley Scales of Infant and Toddler Development was completed.
Results: There were multiple significant differences in demographic (i.e., gestational age) and clinical characteristics (i.e., days without feeds, days on antibiotics, rates of bronchopulmonary dysplasia, length of hospitalization, and postmenstrual age at discharge) between the fentanyl exposure and control groups (Table 1).
Microbiome richness was significantly negatively associated with increased length of fentanyl exposure during hospitalization (adjusted p=0.02, Figure 1). The decreased richness was correlated with a specific deficit in Bacteroidia and changes in multiple metabolites.
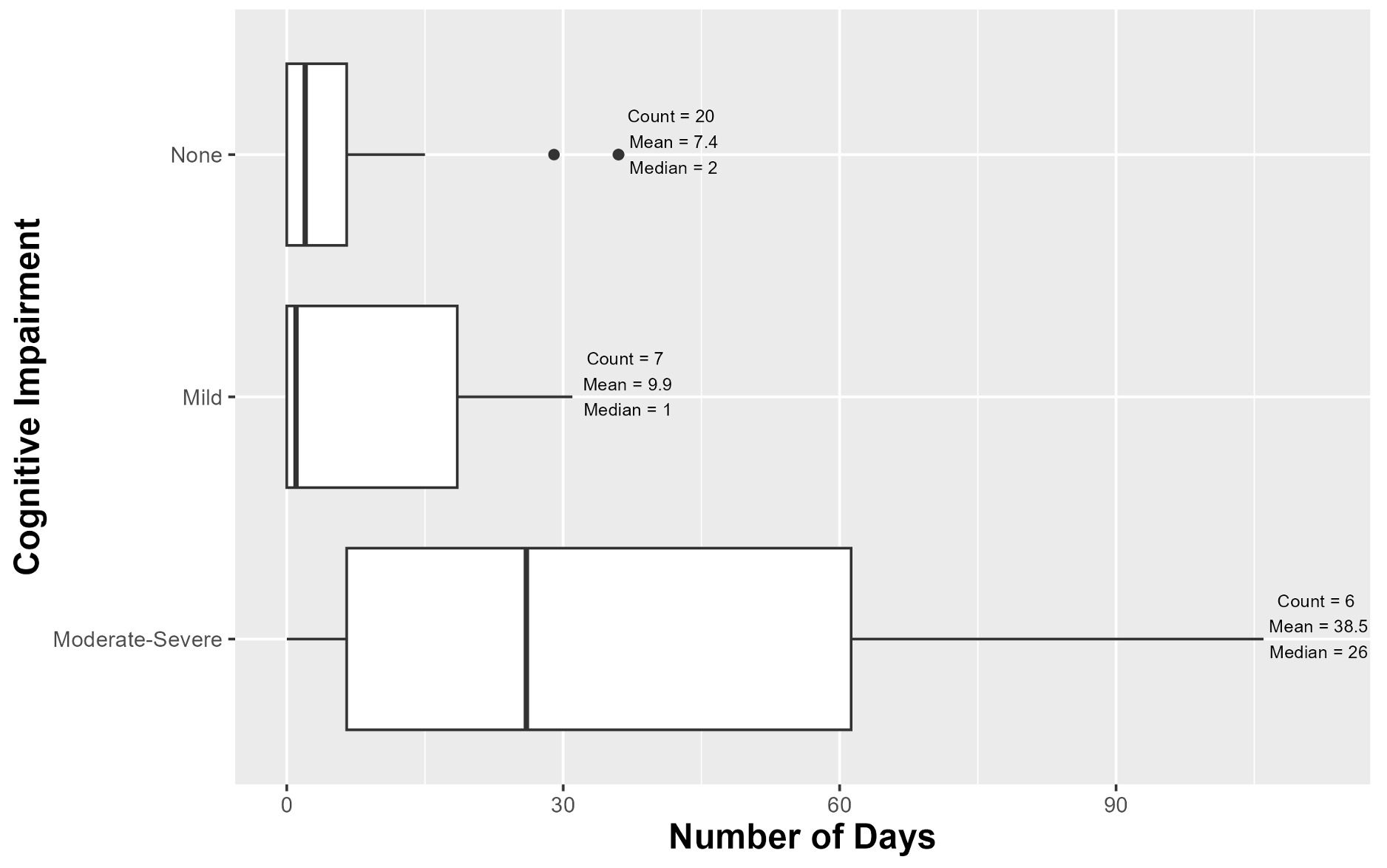
The cognitive domain of the Bayley Scales of Infant and Toddler Development was significantly negatively associated with increased length of fentanyl exposure (p=0.02, Figure 2). However, there was no statistically significant difference for acute fentanyl dose or fentanyl vs. control groups for the Bayley tests when adjusted for confounders.
Conclusion(s): Increased duration of postnatal fentanyl exposure in preterm infants is associated with both short-term decreased gut microbiome richness and later cognitive impairment at 24 months of age.
Table 1: Cohort Demographics, Growth, and Clinical Characteristics
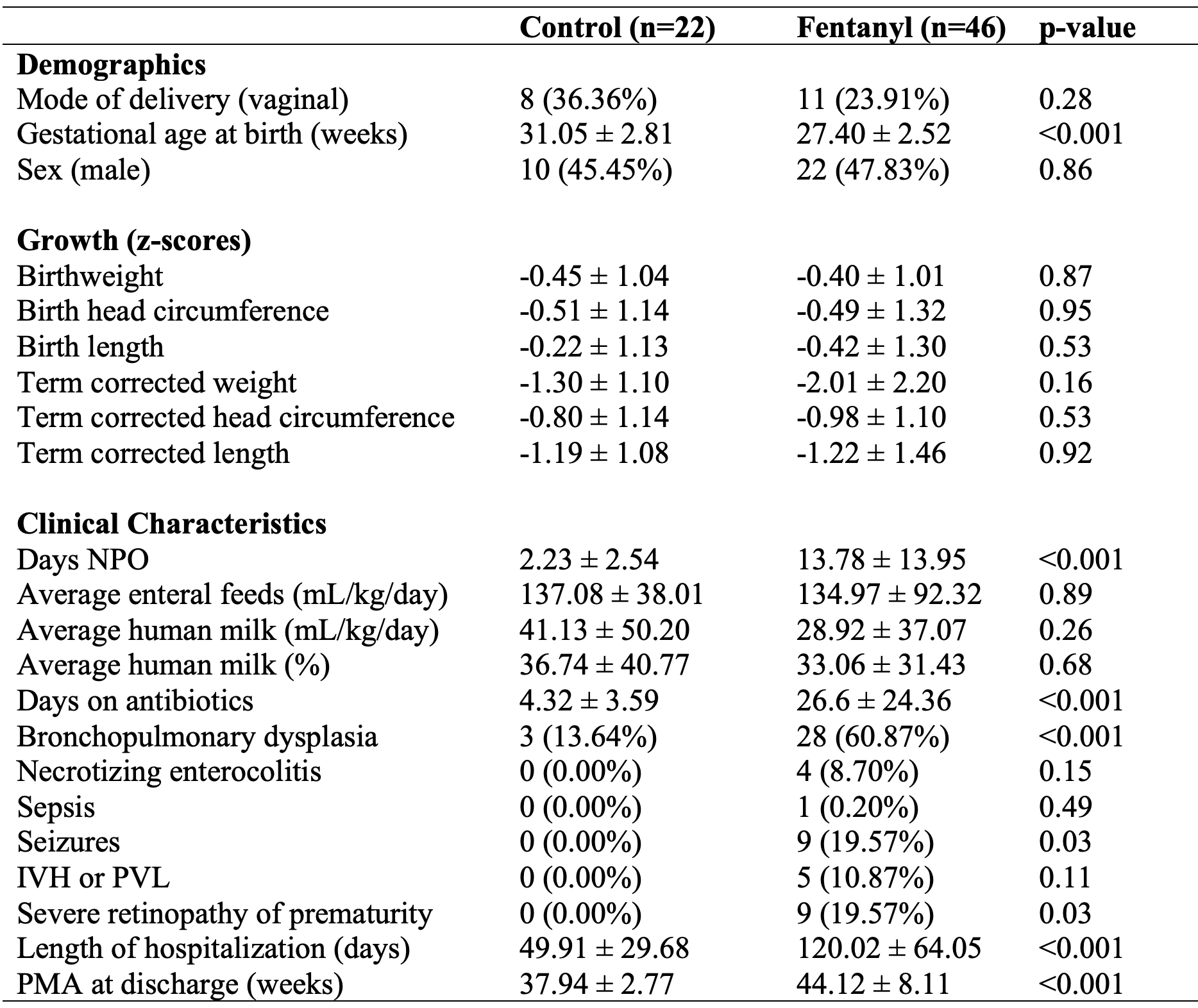
Figure 1: Increased Fentanyl Exposure Associated with Decreased Fecal Richness in the NICU
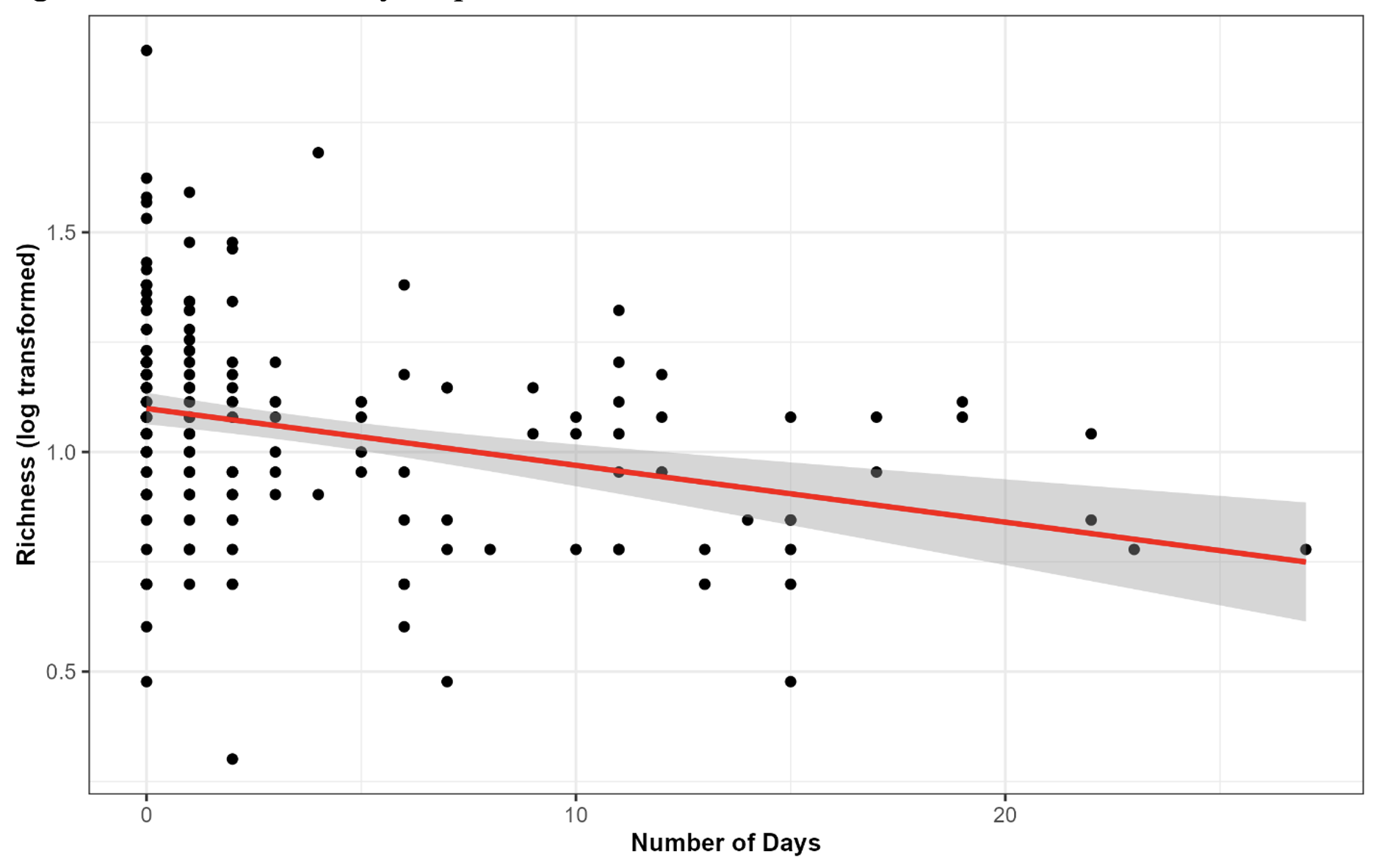
Figure 2: Increased Fentanyl Exposure in the NICU Associated with Cognitive Impairment on the Bayley Scales of Infant and Toddler Development at 24 Months