Neonatal Fetal Nutrition & Metabolism 1
Session: Neonatal Fetal Nutrition & Metabolism 1
614 - Impact of a Nutritional Intervention Program on the Growth Patterns of Infants with Congenital Diaphragmatic Hernia
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 614.5512
Valeria De Toro, Pontificia Universidad Catolica de Chile, Santiago de Chile, Region Metropolitana, Chile; Claudia Garrido, Hospital Clinico UC Christus, Santiago, Region Metropolitana, Chile; Grisell Villarreal, Hospital del Niño Dr. José Renán Esquivel, Ciudad De Panama, Panama, Panama; Matias Luco, Pontificia Universidad Católica de Chile, Santiago, Region Metropolitana, Chile

Valeria De Toro, MD (she/her/hers)
Instructor
Pontificia Universidad Catolica de Chile
Santiago de Chile, Region Metropolitana, Chile
Presenting Author(s)
Background: Congenital diaphragmatic hernia (CDH) is one of the most challenging neonatal diseases with high morbidity, mortality, and frequent nutritional complications. There is limited evidence to support specific nutritional management that determines better results for this complex population.
Objective: To assess the impact of a nutritional intervention program between two periods P1-Pre-intervention (2018-2020) and P2-Post-intervention (2021-2023) on the growth trajectories of infants with CDH during hospitalization.
Design/Methods: Retrospective cohort study including infants with CDH repaired in our center. The nutritional intervention program was performed after 2021 and included progressive caloric-protein intake by increasing caloric density from 0.67 to 0.77/mL from 100 ml/kg/day of enteral intake, followed by individualized follow-up and adjustment. We analyzed the association of growth patterns (weight, length, and head circumference) with daily caloric and protein adjusted by disease-associated severity factors between both periods.
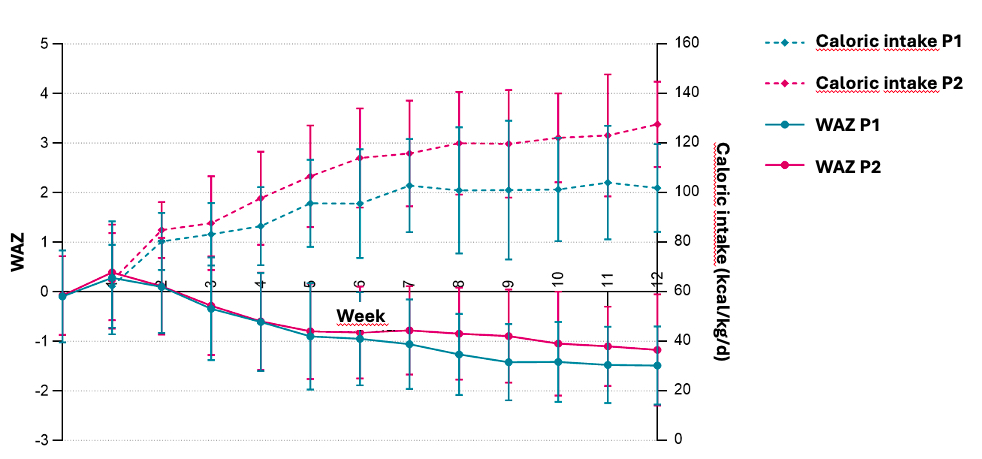
Results: A total of 117 infants were included in this study, 56 (47.9%) in P1 and 61 (52.1%) in P2. There were no differences in baseline characteristics. During hospitalization when full enteral intake was achieved, mean enteral caloric intakes at P1 were 89 ± 38 vs. P2 111 ± 32 kcal/kg/day, p< 0.000, and at discharge P1 101 ± 18 vs. P2 121 ± 18 kcal/kg/day, p< 0.000, Figure 1. A decrease in growth patterns (from birth to discharge) was observed in both periods. However, weight‐for‐age (ΔWAZ) and length-for-age (ΔLAZ) z‐score deltas had significantly smaller decrease at P2 (ΔWAZ -0.98 ± 0.76 and ΔLAZ -1.40 ± 1.05) compared to P1 (ΔWAZ -1.30 ± 0.64, p=0.015 and ΔLAZ -1.85 ± 1.22, p=0.033), with no differences in weight‐for‐length and head circumference‐for‐age. At P1 the frequency of WAZ≤-2.0 increased fivefold from 5.4 to 26.8 %, compared to P2, which increased fourfold from 3.3 to 13.1%. No association was found with protein intake, other nutritional practices, and disease-associated severity factors.
Conclusion(s): The implementation of a nutritional intervention program improves caloric intake and malnutrition in infants with CDH between birth and hospital discharge, independent of disease severity.
Weight-for-age z-score (WAZ) and mean enteral calorie intake at P1 and P2 (birth to discharge)