Infectious Diseases 3: Acute respiratory infections
Session: Infectious Diseases 3: Acute respiratory infections
132 - A Unique Respiratory Syncytial Virus Seasonality Exists in Hawaii
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 132.3932
Arianna M. Antoku, Hawaii Pacific Health, Honolulu, HI, United States; Chieko Kimata, Hawaii Pacific Health, Honolulu, HI, United States; Natascha Ching, University of Hawaii, John A. Burns School of Medicine, Kapiolani Medical Center for Women & Children, Honolulu, HI, United States

Arianna M. Antoku (she/her/hers)
Research Specialist
Hawaii Pacific Health
Honolulu, Hawaii, United States
Presenting Author(s)
Background: Respiratory syncytial virus (RSV) infections are known to cause mild to moderate disease in young children. RSV season occurs from October to March with preventative strategies timed with the season to prevent severe disease in high-risk patients and more recently, all infants under 8 months of age. The Center for Disease Control (CDC) has reported that Hawaii and other locations experience varied RSV seasonal patterns.
Objective: To identify the RSV seasonality and trends in the pediatric patient population in Hawaii.
Design/Methods: A retrospective study was performed to assess RSV seasonality in Hawaii among pediatric patients at Kapiolani Medical Center for Women & Children and Wilcox Memorial Hospital. Pediatric RSV-positive tests were analyzed for hospitalizations and emergency department visits.
Results: We identified trends showing RSV-positive tests in Hawaii appear earlier than the typical season on the continental US. In Hawaii, RSV cases are detected earlier, in August, with peak pediatric cases between October and November prior to the Coronavirus disease 2019 (COVID-19) pandemic. Additionally, RSV cases in Hawaii often persist beyond the usual end of the season in March and are observed year-round—contrary to the October to March seasonality on the continental US. During the COVID-19 pandemic, RSV infections were not detected, consistent with trends across the US. However, as COVID-19 pandemic restrictions eased, RSV infections were detected with greater frequency in pediatric hospitalizations and emergency department visits. The highest RSV peak, post-COVID-19, occurred between September and November 2022. After the COVID-19 pandemic, including the time after the end of the public health emergency, RSV-positive tests were detected in greater numbers. This rise in RSV-positive tests may reflect either increased circulation or increased detection due to expanded testing capability rather than solely relying on stand-alone RSV tests.
Conclusion(s): RSV circulation in Hawaii does not follow a classic seasonal pattern and generally persists at low to moderate levels, even after the season concludes on the continental US. RSV preventative strategies for pediatric patients differ from those on the continental US, based on the recent recommendations from the Hawaii Department of Health and CDC for year-round consideration. In Hawaii, continued monitoring of RSV seasonality and potential change in patterns is important as RSV immunization of pregnant persons and RSV prophylaxis strategies are implemented.
Pediatric RSV in Hawaii
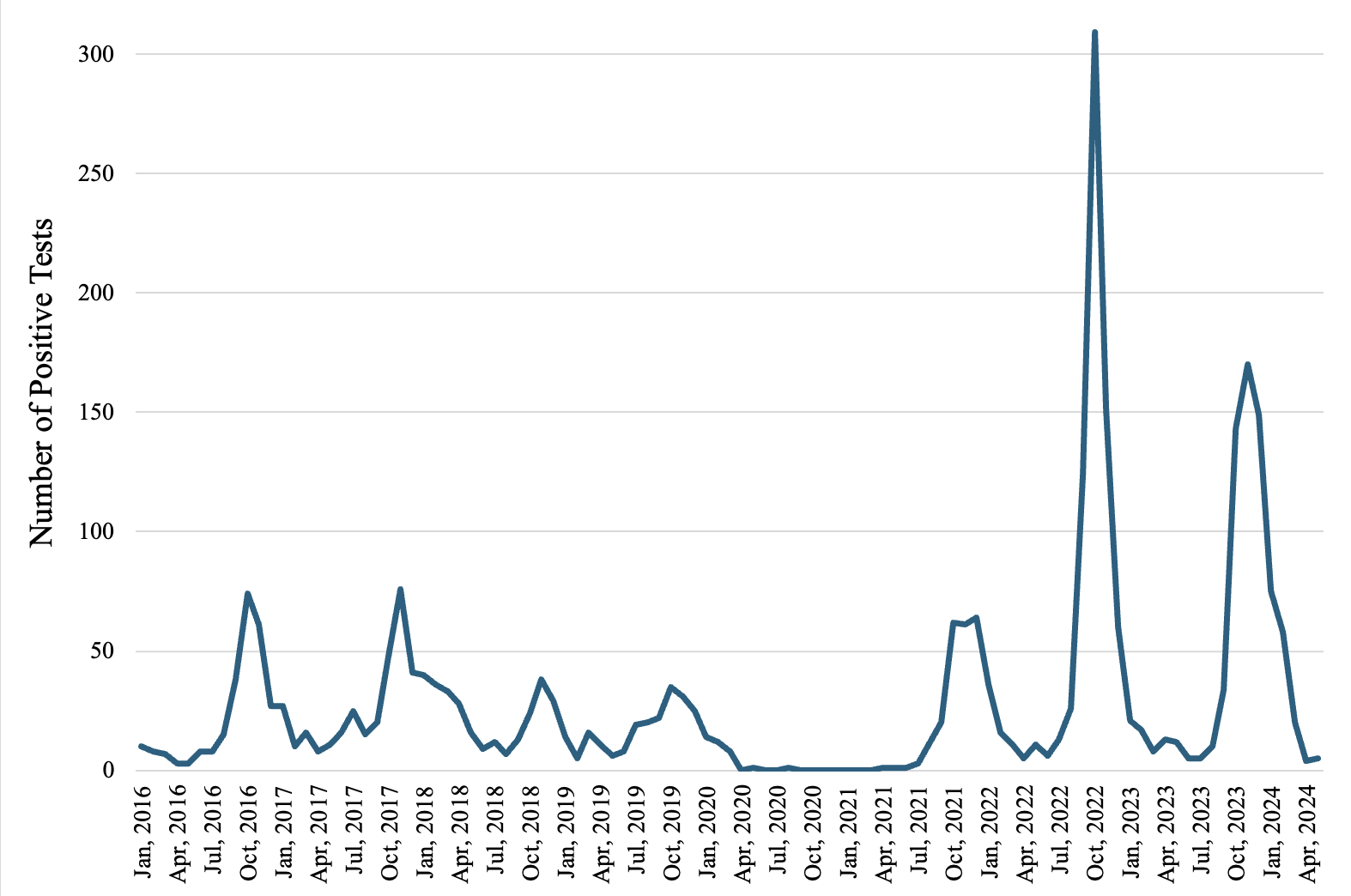 Figure 1. Pediatric RSV in Hawaii—combined positive-RSV tests from hospitalized and emergency department visits.
Figure 1. Pediatric RSV in Hawaii—combined positive-RSV tests from hospitalized and emergency department visits.
