Neonatal GI Physiology & NEC 1
Session: Neonatal GI Physiology & NEC 1
715 - Are Growth Restricted Preterm Neonates at Higher Risk of Adverse Outcomes Post-surgical Necrotizing Enterocolitis ? : A Retrospective Cohort Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 715.3930
Ujjwala Mantha, The Hospital for Sick Children, Toronto, ON, Canada; Dwayne Mascarenhas, The Hospital for Sick Children, Toronto, ON, Canada; Shravan Kanaparthi, The Hospital for Sick Children, Toronto, ON, Canada; Doaa Al-Dweik, The hospital of Sick Children, Toronto, ON, Canada; Jordan Mann, The Hospital for Sick Children, Toronto, ON, Canada; Telford Yeung, University of Calgary, Calgary, AB, Canada; Mary A. Woodward, The Hospital for Sick Children, Toronto, ON, Canada; Bonny Jasani, The Hospital for Sick Children, Toronto, ON, Canada
- UM
Ujjwala Mantha, MD (she/her/hers)
Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Small for gestational age [SGA: Birth weight < 10%tile for gestational age (GA)] neonates are prone to adverse perinatal outcomes due to the "brain-sparing" effect, which prioritizes blood flow to the brain over the gastrointestinal system. This redistribution may lead to reduced blood flow to the intestinal mucosa potentially increasing the risk for necrotizing enterocolitis (NEC), especially in preterm neonates. Limited data exists regarding outcomes for preterm SGA neonates post-surgical NEC (sNEC).
Objective: To evaluate the mortality, morbidities and short-term outcomes in SGA versus appropriate for gestational age (AGA) preterm neonates recovering from sNEC.
Design/Methods: We conducted a retrospective cohort study of preterm neonates < 30 weeks gestation with sNEC at a single quaternary neonatal intensive care unit between January 2016 to June 2024. The pre-specified outcomes included post-procedural complications, the need for additional laparotomy, neonatal morbidities, and anthropometric indices (weight, length, head circumference z-scores) at 36 weeks postmenstrual age (PMA). Mann-Whitney U test and Fisher’s exact test were used for comparing continuous and categorical data respectively between the two groups.
Results: Over the study period a total of 139 preterm neonates [SGA (n=23) and AGA (n=116)] with sNEC were included. Baseline characteristics were similar between the groups (Table 1). The preoperative assessment showed a significantly lower platelet count in the SGA group (p=0.0023). Compared to AGA neonates with sNEC, moderate-severe BPD and BPD-PH were more common in the SGA group (p=0.035 and 0.001, respectively). SGA babies had significantly lower Z scores for weight and HC at 36 weeks PMA (Table 2). MLR analysis revealed higher unadjusted odds of BPD, BPD-PH and lower HC z-scores in sNEC among preterm SGA neonates; however, after adjustment, these outcomes were not significant (Table 3).
Conclusion(s): Our single-centre study showed that small for gestation preterm neonates with surgical necrotizing enterocolitis had comparable short-term outcomes to appropriate for gestational age neonates.
Table 1: Baseline characteristics, pre-operative and details of surgical intervention in preterm small for gestation neonates with surgical necrotizing enterocolitis
.jpg) Abbreviations: PPROM: Premature prolonged rupture of membranes.
Abbreviations: PPROM: Premature prolonged rupture of membranes.Table 2: Post-surgical mortality, morbidities and short-term outcomes
.jpg) Abbreviations: BPD-PH: bronchopulmonary dysplasia associated pulmonary hypertension, NEC: Necrotizing enterocolitis, NIV: Non-invasive ventilation, PMA: Post menstrual age, PNALD: Parenteral nutrition associated liver disease, ROP: Retinopathy of prematurity.
Abbreviations: BPD-PH: bronchopulmonary dysplasia associated pulmonary hypertension, NEC: Necrotizing enterocolitis, NIV: Non-invasive ventilation, PMA: Post menstrual age, PNALD: Parenteral nutrition associated liver disease, ROP: Retinopathy of prematurity.Table 3: Association between SGA and pre-specified neonatal outcomes in surgical NEC
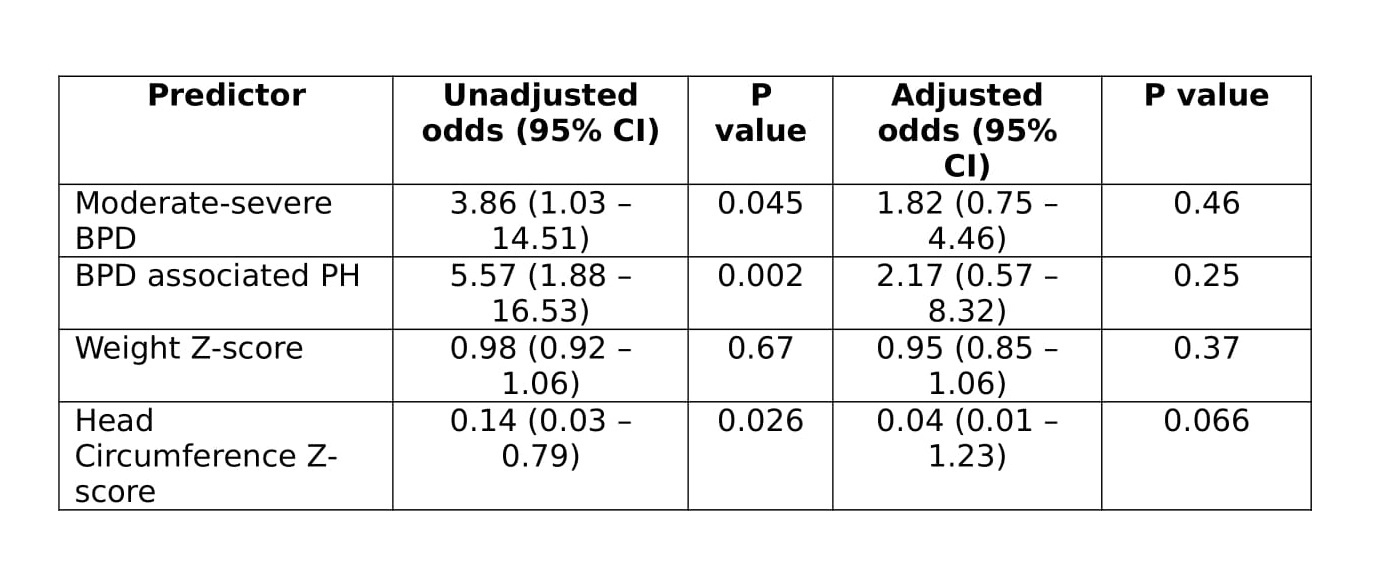 BPD – bronchopulmonary dysplasia, CI – confidence interval, PH – pulmonary hypertension
BPD – bronchopulmonary dysplasia, CI – confidence interval, PH – pulmonary hypertensionCovariates were birth weight and lowest platelet count in the 48-hour pre-operative period.

