Neonatal Fetal Nutrition & Metabolism 1
Session: Neonatal Fetal Nutrition & Metabolism 1
611 - Association between time NPO and body composition in VLBW infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 611.3989
Gregory P. Goldstein, Tufts University School of Medicine, Boston, MA, United States; Volha Belavusava, Tufts Childrens Hospital, Quincy, MA, United States; Rachana Singh, Tufts University School of Medicine, Boston, MA, United States; Olivia Marchioni, Tufts Childrens Hospital, Boston, MA, United States

Gregory P. Goldstein, MD, MS
Assistant Professor of Pediatrics
Tufts University School of Medicine
Boston, Massachusetts, United States
Presenting Author(s)
Background: Postnatal growth restriction and less lean body mass in preterm infants are associated with increased risk of adverse neurodevelopmental outcomes. Fat-free mass (FFM) may be more suitable than body weight to assess quality of growth during the NICU hospitalization. Higher protein and energy intake during a critical early period in development is advantageous for preterm infant growth because it increases weight gain, weight z-score and FFM accretion. It is unclear whether minimizing time receiving no enteral feeds (i.e. nothing per mouth or NPO) impacts body composition in preterm infants.
Objective: The objective of this study was to determine the association between time NPO and body composition in VLBW infants.
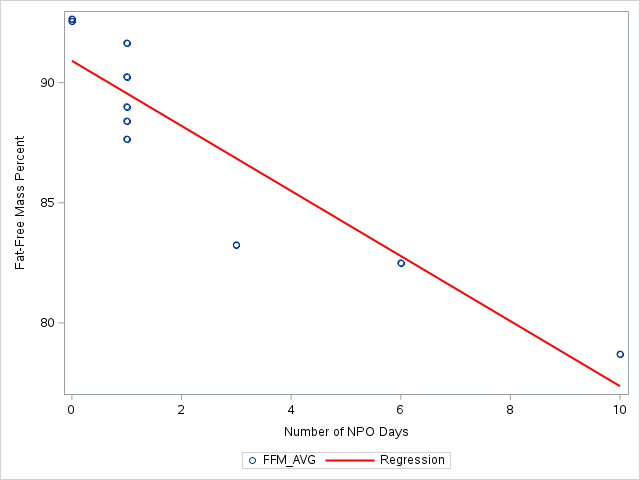
Design/Methods: VLBW infants < 32 weeks gestational age (GA) or < 1500 grams at birth were prospectively enrolled from the Tufts Medical Center NICU and underwent air displacement plethysmography (ADP) near time of NICU discharge to measure body composition. Patient characteristics were assessed including prenatal medical and sociodemographic factors, postnatal clinical factors, and ADP measurement data, which included FFM and fat mass (FM) percentage. Multivariable regression models were used to estimate the association between number of days NPO and FFM.
Results: 10 infants were enrolled with an average birth GA of 29.2 weeks (standard deviation 3.3) and birth weight of 1155 grams (SD 369). Body composition measurement was performed on average at 37.7 weeks corrected gestational age. Infants received full volume enteral feeds for an average of 80% of their NICU hospitalization and were NPO for 2.9%. Average FFM was 87.7% (SD 4.7), FM 12.3% (SD 4.7), and NICU discharge weight z-score was -1.13 (SD 0.69). Infants with lower FFM were more likely to have lower gestational ages at birth, major morbidities including bronchopulmonary dysplasia, persistent PDA and sepsis, and longer hospitalizations. After adjusting for confounding variables, number of days NPO was negatively associated with FFM (p=0.03).
Conclusion(s): Decreased fat-free mass is associated with longer time NPO during the NICU hospitalization. Time NPO may negatively impact body composition in VLBW infants. More research is needed to understand how to use nutrition during the NICU hospitalization to improve body composition in VLBW infants.
Scatterplot of Time NPO and Fat-Free Mass