Neonatal General 5: Infectious Disease and Immunology
Session: Neonatal General 5: Infectious Disease and Immunology
149 - Enlarged Subarachnoid Space in Very Low Birth Weight Infants with Neonatal Sepsis
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 149.4854
Patricia Moran, UVA, Charlottesville, VA, United States; Ari Esrig, University of Virginia School of Medicine, Charlottesville, VA, United States; Emma Hostetter, University of Virginia School of Medicine, Charlottesville, VA, United States; Gabrielle Mazzoni, University of Virginia School of Medicine, Charlottesville, VA, United States; Brynne Sullivan, University of Virginia School of Medicine, Charlottesville, VA, United States; Jennifer Burnsed, University of Virginia School of Medicine, Charlottesville, VA, United States; santina Zanelli, University of Virginia School of Medicine, Charlottesville, VA, United States

Patricia Moran, MD (she/her/hers)
Neonatology Fellow
UVA
Charlottesville, Virginia, United States
Presenting Author(s)
Background: Sepsis is a common morbidity after premature birth. Both the infection and associated systemic inflammation can cause brain injury, particularly of the white matter, which is best assessed using brain MRI. Enlargement of the subarachnoid space (ESS), defined as a sinocortical width (SCW) > 3.5 mm on head ultrasound, is being studied as a surrogate marker of white matter volume loss. Recent evidence suggests that the presence of ESS is associated with developmental delays in preterm infants. If confirmed, ESS could represent a useful biomarker of adverse outcome risk. Whether ESS occurs in very low birth weight (VLBW) infants with sepsis has not been previously described.
Objective: To determine the prevalence of ESS in VLBW infants with culture-positive sepsis, culture-negative sepsis, and in VLBW infants without sepsis.
Design/Methods: Single center, retrospective cohort study evaluating the incidence of ESS in VLBW infants with culture-positive sepsis, culture-negative sepsis, and no sepsis. Medical records were reviewed for mode of delivery, antenatal steroids, infant characteristics, including gestational age (GA), birth weight, sex, race, ethnicity, pathogens identified on blood, urine, and CSF cultures, diagnosis of necrotizing enterocolitis (NEC), and head ultrasound findings, including the highest degree of IVH. Infants were categorized into one of three cohorts: (1) culture-proven sepsis (bacteremia, UTI, meningitis, NEC); (2) culture-negative sepsis (antibiotics > 48h); and (3) no sepsis (no antibiotics received or ≤48h). Head ultrasounds at 36 weeks postmenstrual age (PMA), or closest to discharge, whichever was later, were reviewed. The SCW was measured by four reviewers. Infants who did not have a head ultrasound at ≥35 weeks PMA were excluded.
Results: Preliminary data in 120 VLBW infants born between 2019 and 2022 was collected (39% culture-positive sepsis, 23% culture-negative, 38% without sepsis). Maternal and infant characteristics are shown in Table 1. ESS was present in 32% of infants with culture-positive sepsis compared to 33% in the culture-negative cohort and 9% in the cohort without sepsis, (p<=0.019, ANOVA, see Fig. 1 for representative examples).
Conclusion(s): ESS is more common in VLBW infants with culture-positive and culture-negative sepsis compared to those without a diagnosis of sepsis. Analysis is ongoing to complete assessment of ESS in the entire cohort of 600 VLBW infants. Work is also ongoing to evaluate intra- and inter-rater reliability of ESS measurements. Future research will focus on exploring the prognostic value of ESS diagnosis in preterm infants.
Figure 1: Representative infant with and without ESS on head ultrasound
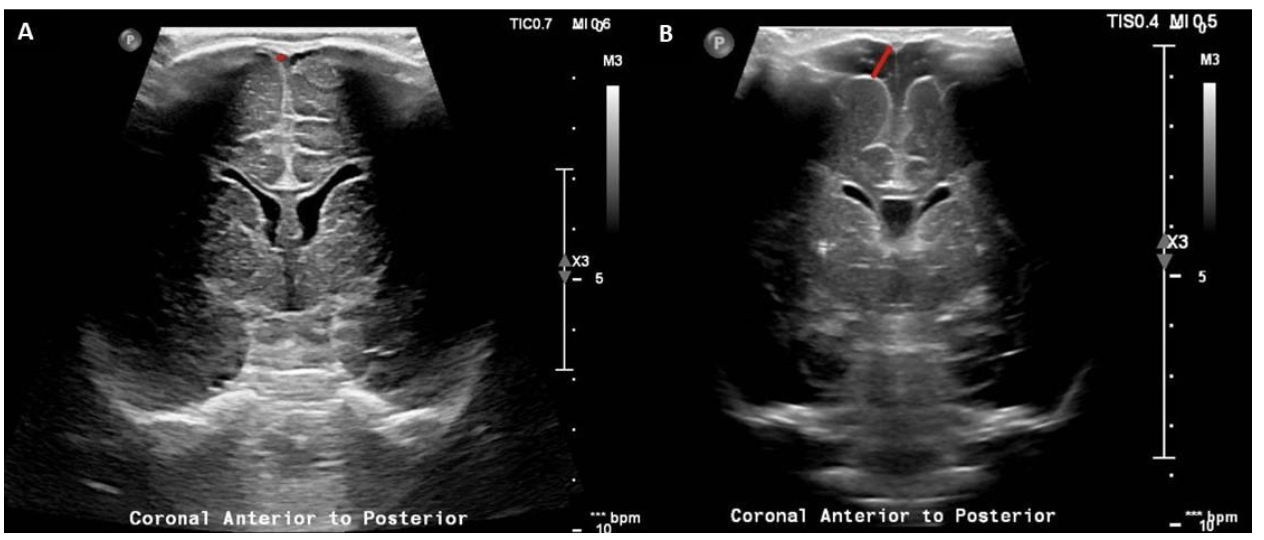 Panel A: Linear coronal view of a head ultrasound obtained at 44 weeks PMA in an infant born at 25 5/7 weeks and with a history of E-Coli early onset sepsis. SCW was measured to be 0.99 mm. Panel B: Linear coronal image of a head ultrasound obtained at 35 6/7 weeks PMA in an infant born at 25 6/7 weeks and with a history of Klebsiella late onset sepsis. SCW was measured to be 6.23 mm. Of note, all the measurements of SCW were obtained at the level of the foramen of Monro for standardization.
Panel A: Linear coronal view of a head ultrasound obtained at 44 weeks PMA in an infant born at 25 5/7 weeks and with a history of E-Coli early onset sepsis. SCW was measured to be 0.99 mm. Panel B: Linear coronal image of a head ultrasound obtained at 35 6/7 weeks PMA in an infant born at 25 6/7 weeks and with a history of Klebsiella late onset sepsis. SCW was measured to be 6.23 mm. Of note, all the measurements of SCW were obtained at the level of the foramen of Monro for standardization.Table 1: Infant and Maternal Demographics
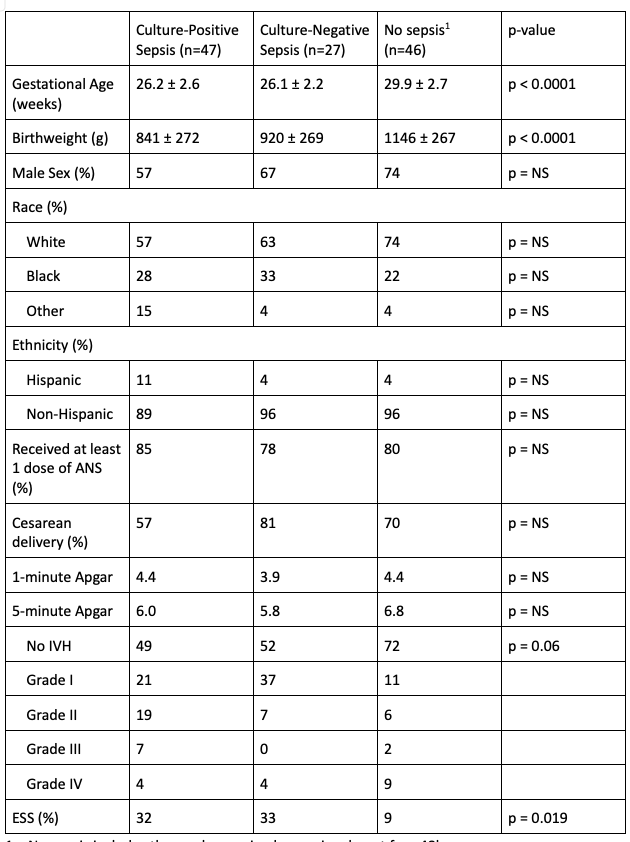 1 – No sepsis includes those who received a sepsis rule out for <48h.
1 – No sepsis includes those who received a sepsis rule out for <48h. ANOVA was used to compare means across groups and chi-square with Fisher’s exact test was used for categorical variables
Legend: ESS = enlarged subarachnoid space, ANS = antenatal steroids

