Emergency Medicine 5
Session: Emergency Medicine 5
273 - Using Feedback From Paediatric Resuscitation Team Members To Improve Quality Of Care
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 273.7033
Erin Mills, Monash Health, Melbourne, Victoria, Australia; Shameera Navaratnam, Monash Medical Centre and Ministry of Health Malaysia, Federal Territory of Kuala Lumpur, Kuala Lumpur, Malaysia; Clifford J. Connell, Monash University, Somers, Victoria, Australia; Harshika Herath, Monash University, Clayton, Victoria, Australia; Phyllis Lin, Monash University, Box Hill, Victoria, Australia; Annmarie Bermundo, Monash, West End, Queensland, Australia; Celia Bagshaw, Monash Medical Centre, Clayton, Victoria, Australia; Tobias van Hest, Monash University, Clayton, Victoria, Australia; Adam West, Monash Health, Clayton, Victoria, Australia; Jessica L. Nooney, Monash Childrens Hospital. Monash University, Melbourne, Victoria, Australia; Simon Craig, Monash University, Clayton, Victoria, Australia

Simon Craig, MBBS FACEM MPH MHPE PhD (he/him/his)
Paediatric Emergency Physician / Adjunct Clinical Professor
Monash Health / Monash University
Clayton, Victoria, Australia
Presenting Author(s)
Background: Paediatric resuscitations in the Emergency Department (ED) are high-pressure situations that occur in a complex and unpredictable environment. Traditionally only resuscitations with a poor outcome are reviewed in depth, with improvements designed to prevent future failures. However, teams that adopt a Safety-II mindset regularly reflect on their actions and processes and learn from both the positive and negative experiences. This approach has been shown to enhance the quality of care they provide.
Objective: To identify and describe the themes obtained from staff feedback after paediatric resuscitation in the ED, and system changes implemented as a result of this feedback.
Design/Methods: A prospective quality improvement study was conducted in which surveys were emailed to clinical staff involved in paediatric resuscitations within the ED. The surveys requested feedback on what went well and suggestions for improving care for the next similar patient. Responses were analysed using directed content analysis: initially coded using the London Protocol, a systems-focused review methodology, followed by inductive thematic analysis. Feedback was discussed in departmental Mortality and Morbidity, and Quality and Safety Meetings, leading to the initiation of clinical improvements to enhance patient care.
Results: A total of 89 paediatric resuscitation cases were identified, with a median of 9 feedback request emails sent per resuscitation and a median 3 replies. 1320 specific items of feedback were received from 256 staff members. Feedback covered all layers of the health system, with the most common themes relating to the team, the environment and tasks and technology. The feedback informed the design and implementation of a number of systemic improvements, including development of a transport checklist, initiation of a start of shift airway huddle, and the standardisation medication preparation methods.
Conclusion(s): Asynchronous feedback from staff involved in paediatric resuscitations identified positive and constructive themes across all layers of the health system. This feedback was successfully translated into a number of systems-focussed actions to improve patient safety and care.
Table 1
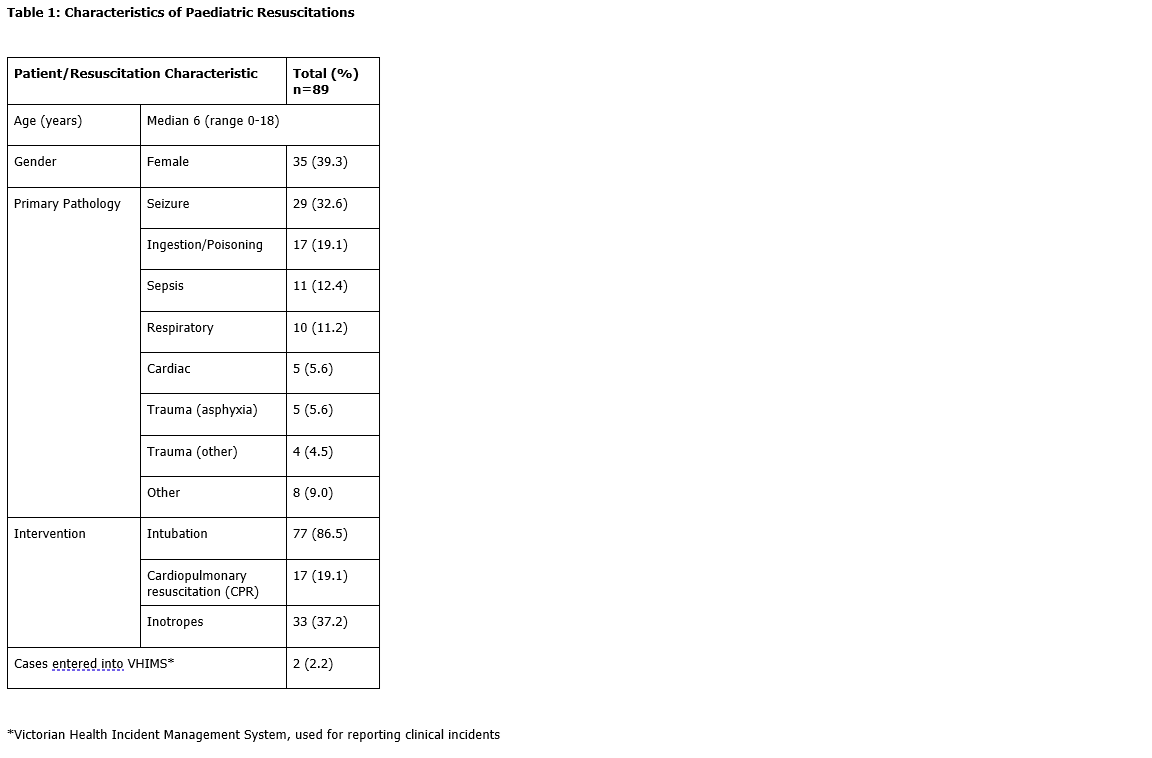 Characteristics of Paediatric Resuscitations
Characteristics of Paediatric ResuscitationsFigure 1
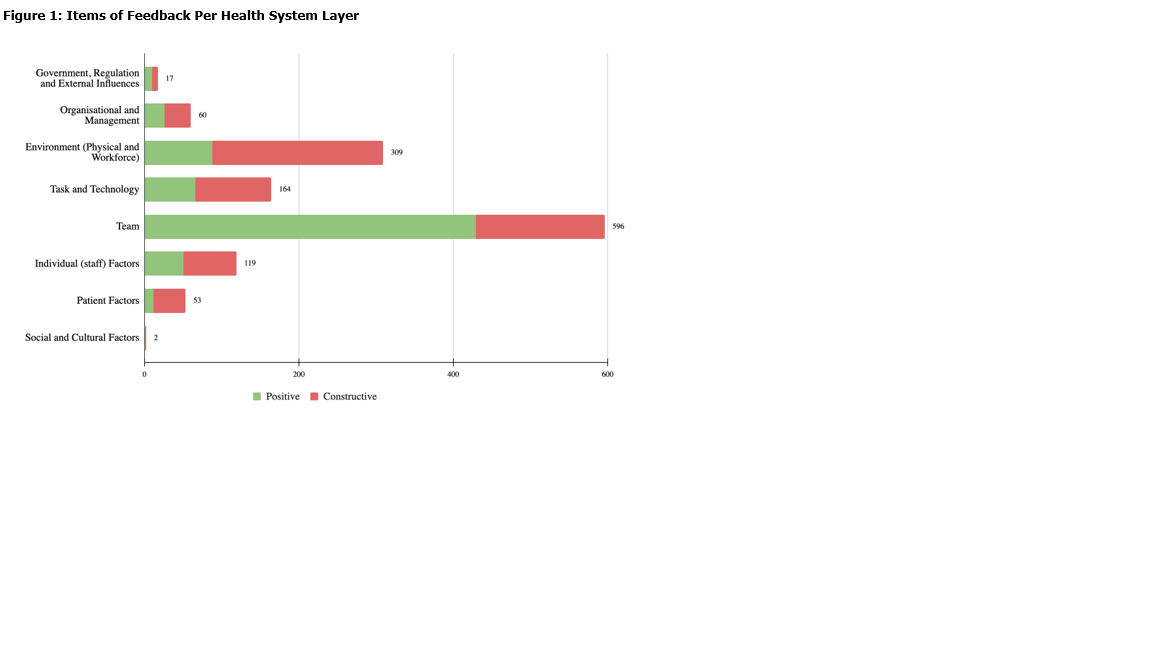 Items of Feedback Per Health System Layer
Items of Feedback Per Health System LayerTable 2
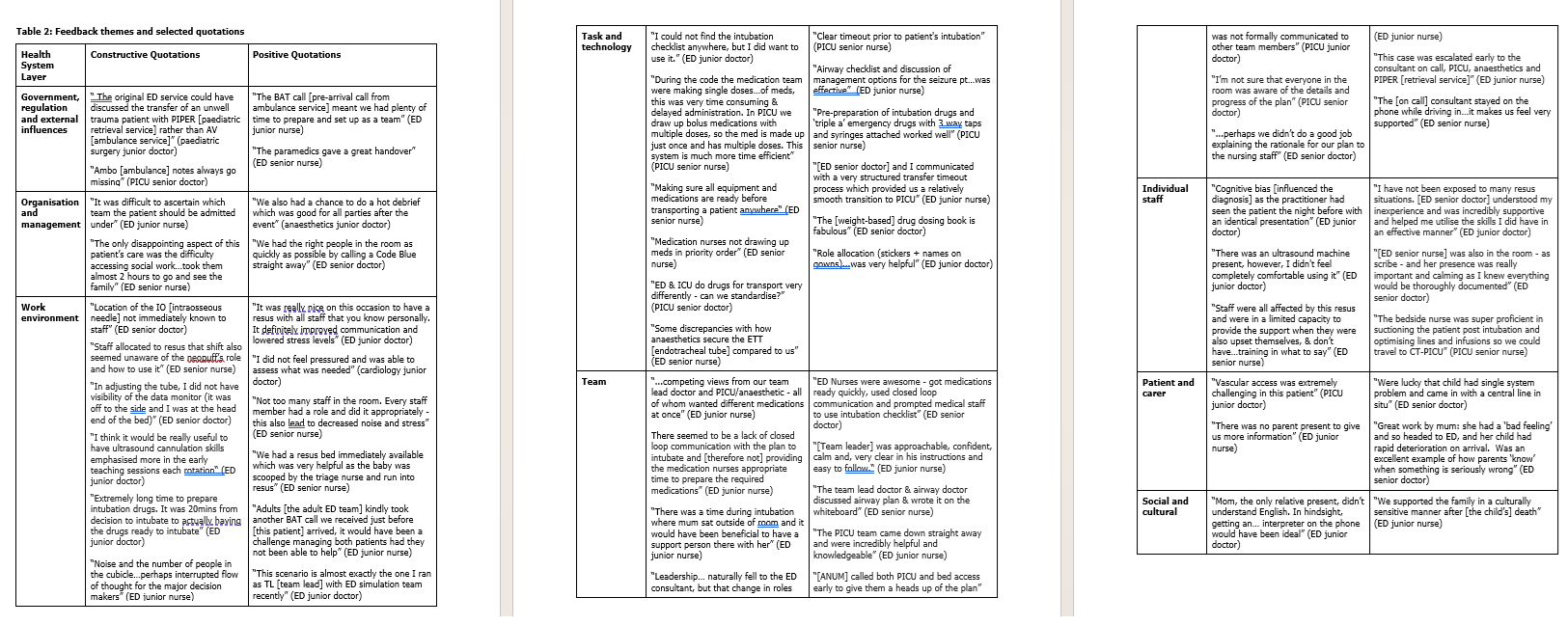 Feedback themes and selected quotations
Feedback themes and selected quotations Table 1
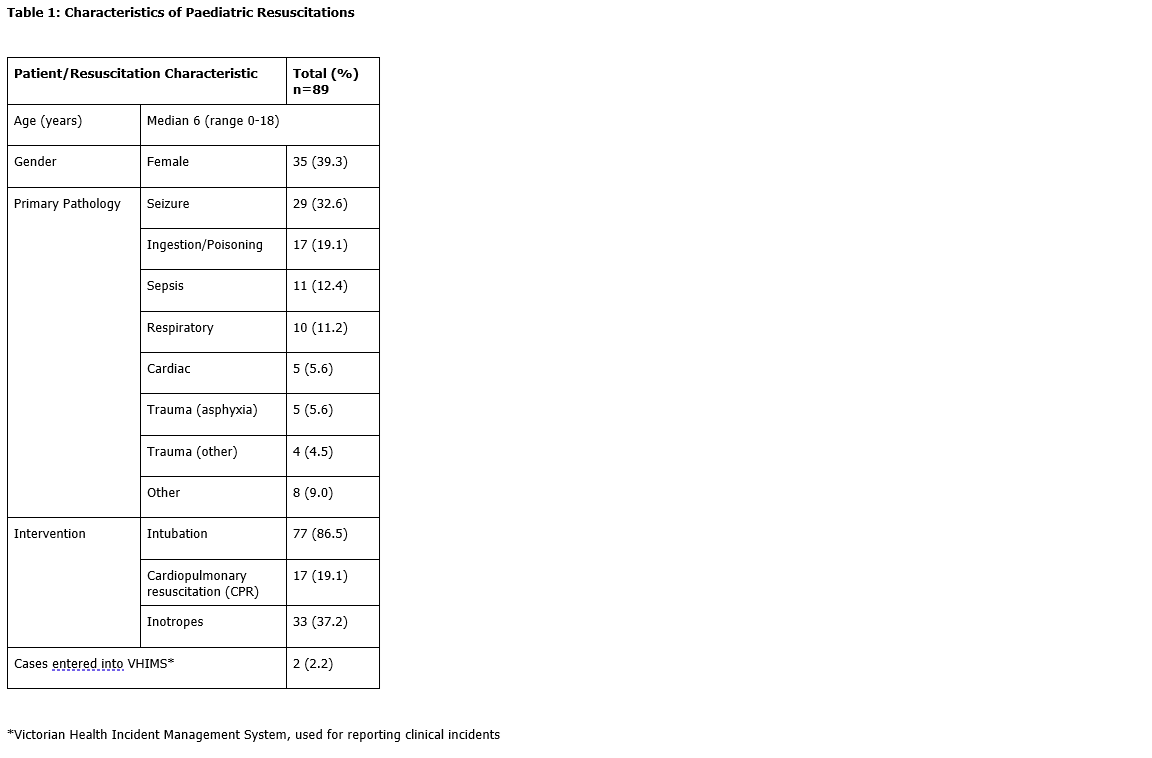 Characteristics of Paediatric Resuscitations
Characteristics of Paediatric ResuscitationsFigure 1
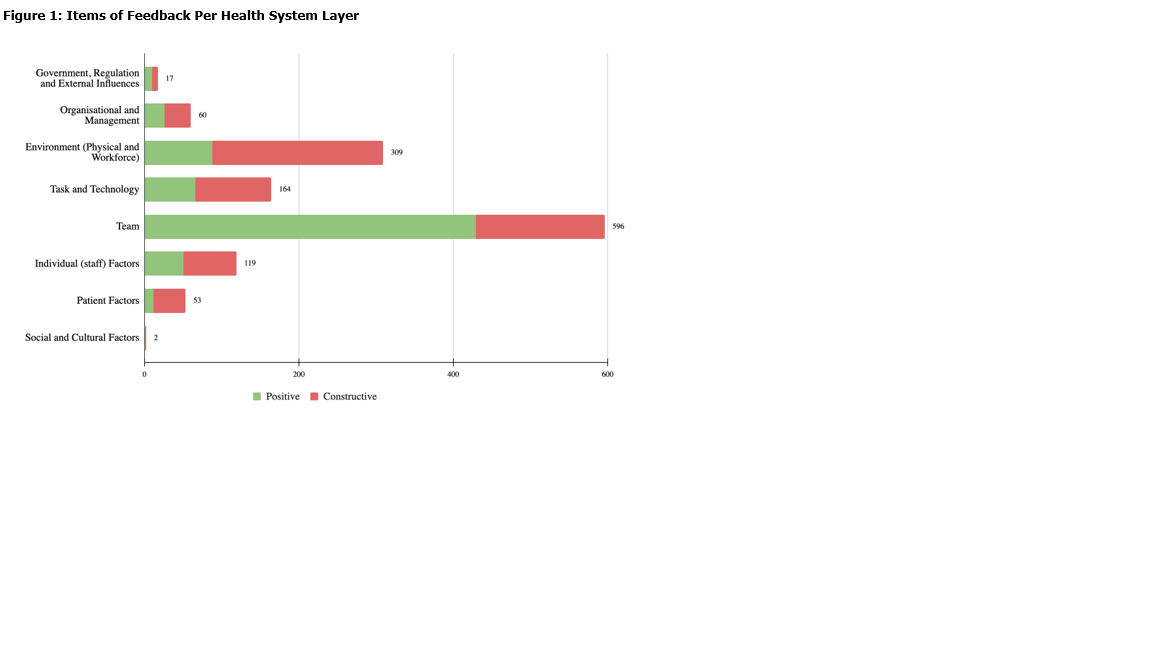 Items of Feedback Per Health System Layer
Items of Feedback Per Health System LayerTable 2
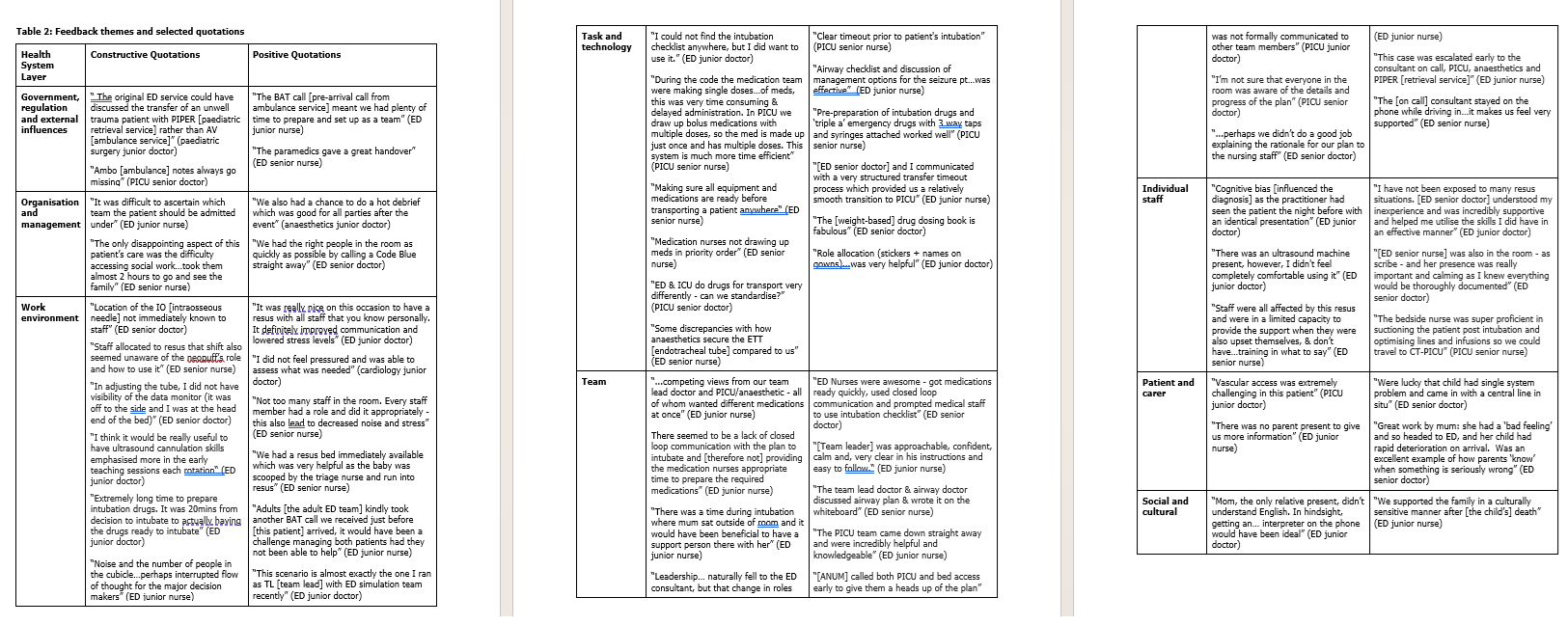 Feedback themes and selected quotations
Feedback themes and selected quotations 
