Neonatal Hemodynamics and Cardiovascular Medicine 4
Session: Neonatal Hemodynamics and Cardiovascular Medicine 4
090 - Utility of multimodal hemodynamic measures to predict intraventricular hemorrhage and mortality in preterm infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 90.7051
Aleksandra M. Hibner, University of California, San Diego School of Medicine, Phoenix, AZ, United States; Lin Liu, University of California, San Diego, la Jolla, CA, United States; Shashank Sanjay, Sharp Health Care, San Diego, CA, United States; Henry C. Lee, University of California, San Diego School of Medicine, La Jolla, CA, United States; Anup Katheria, Sharp Mary Birch Hospital for Women & Newborns, San Diego, CA, United States
- AH
Aleksandra M. Hibner, MD
Fellow
University of California, San Diego School of Medicine
Phoenix, Arizona, United States
Presenting Author(s)
Background: BACKGROUND
Preterm infants are at high risk of morbidity, such as intraventricular hemorrhage (IVH) and death due to adverse hemodynamics. Despite efforts to use various noninvasive modalities to predict and treat abnormal values, outcomes have not improved.
Objective: We aimed to explore whether combining any, some, or all commonly used monitors could enhance the ability to detect IVH or death.
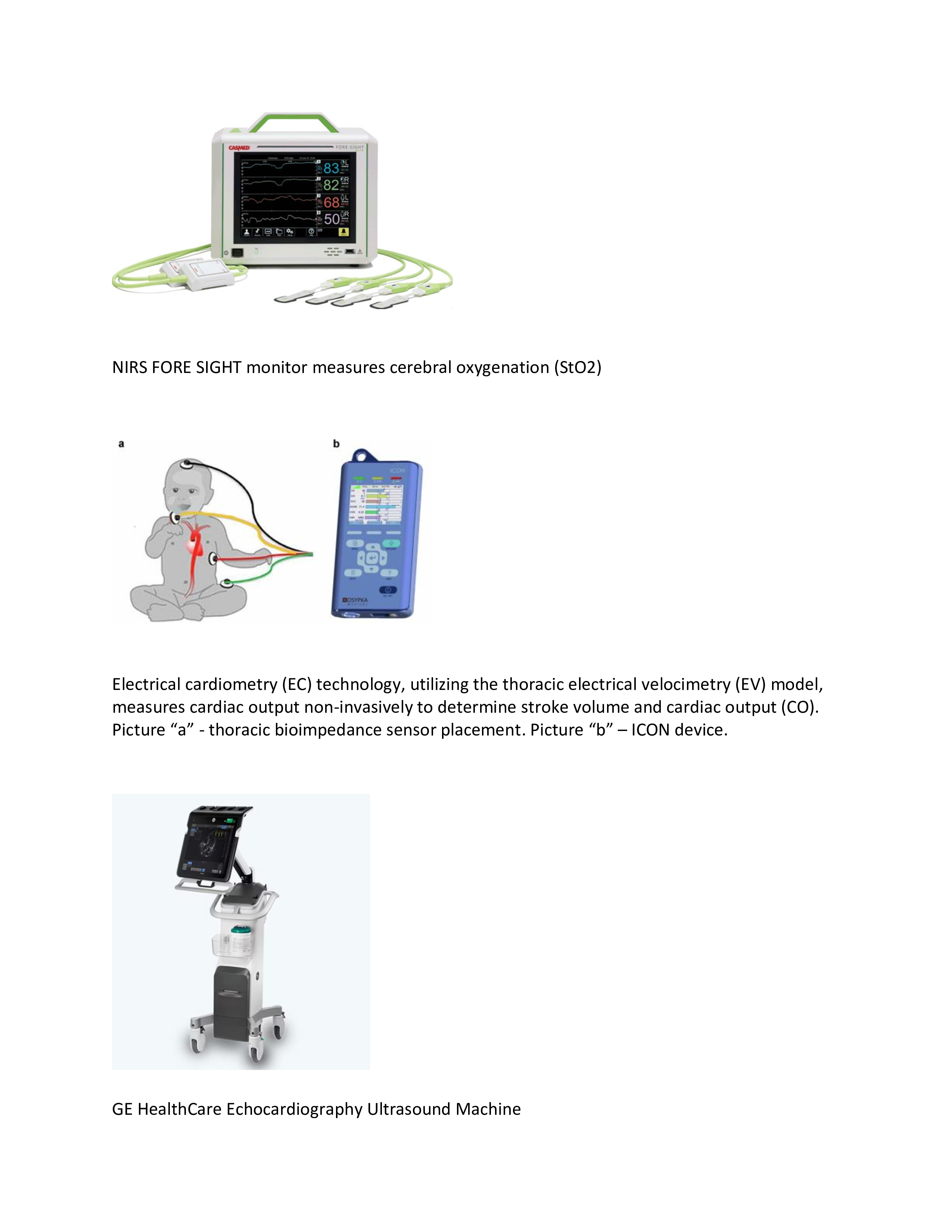
Design/Methods: 482 infants born at less than 32 wks gestational age (GA) with hemodynamic monitoring data, including cerebral oximetry (StO2) measured by near-infrared spectroscopy (NIRS), mean arterial blood pressure (MAP), cardiac output (CO) measured by electrical cardiometry (EC), and measures of systemic blood flow by echocardiography (ECHO), in the first 24 hours of life were included (Figure 1). The primary outcome was whether any monitoring data could predict IVH or death before discharge. Wilcoxon Rank-Sum and chi-squared tests were performed for continuous and categorical variables and group comparisons. Multivariable logistic regression was conducted to identify predictors. ROC was created for each predictor to determine if the optimal cut point best predicts outcomes. Lastly, combinations of any parameters were included to determine if ROCs could improve prediction.
Results: Baseline demographics are shown in Table 1. Among all the unadjusted variables, gestational age (GA) had the highest sensitivity and specificity for predicting IVH and death (Table 2). After adjusting for GA, a one-unit (mmHg) increase in MAP over a 24 h period was associated with an 18.6% decrease in the odds of death (OR = 0.814; 95% CI: 0.679, 0.944; P = 0.013) and a one-unit (ml/kg/min) increase in right ventricular function (RVO) was associated with a 0.4% decrease in the odds of IVH (OR = 0.996; 95% CI: 0.991, 0.999; p-value 0.031). However, a combination of any of these parameters did not improve prediction of IVH or death (data not shown).
Conclusion(s): Integration of multimodal hemodynamic techniques may offer a comprehensive approach to evaluating the risk of IVH and mortality in preterm infants. Despite the availability of continuous cardiac output and cerebral oxygen monitoring (by electrical cardiometry and NIRS, respectively), only right ventricular output and mean arterial blood pressure were predictive of death or IVH, but no combination of these parameters improved detection. Future studies need to consider which modalities could be useful for early interventions in preterm infants at risk for death or IVH.
Baseline demographics.
.jpg) Legend: n= number of subjects, Data reported as mean (%) except gestational age and birth weight (standard deviation). IVH: intraventricular hemorrhage.
Legend: n= number of subjects, Data reported as mean (%) except gestational age and birth weight (standard deviation). IVH: intraventricular hemorrhage.Summary of results of ROC analysis for predictors of IVH and Death.
.jpg) GA: gestational age; MAP: mean arterial pressure; StO2: cerebral oxygenation measures by near-infrared spectroscopy; IVH: Intraventricular hemorrhage; StO2 t min: cerebral oxygenation total time in minutes < 67%; CO: cardiac output based on electrical cardiometry; CO min: duration in minutes of cardiac output < 150 ml/kg/min; SVC: superior vena cave flow; RVO: right ventricular function; LVO: left ventricular function.
GA: gestational age; MAP: mean arterial pressure; StO2: cerebral oxygenation measures by near-infrared spectroscopy; IVH: Intraventricular hemorrhage; StO2 t min: cerebral oxygenation total time in minutes < 67%; CO: cardiac output based on electrical cardiometry; CO min: duration in minutes of cardiac output < 150 ml/kg/min; SVC: superior vena cave flow; RVO: right ventricular function; LVO: left ventricular function.Monitoring devices used in the project.