Emergency Medicine 5
Session: Emergency Medicine 5
270 - Standardization of Rapid-Sequence Intubation to Reduce Time to Post-Intubation Sedation: A Quality Improvement Initiative
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 270.6794
Collin Huth, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Hellene Speicher, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Sajja Vanitha, UH Rainbow Babies & Children's Hospital, Solon, OH, United States; Caitlin Gaffney, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Tracy McCallin, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Dina Dornack, UH Rainbow Babies & Children's Hospital, Akron, OH, United States; Erin Hoehn, UH Rainbow Babies & Children's Hospital, Shaker heights, OH, United States

Collin Huth, MD (he/him/his)
Resident
UH Rainbow Babies & Children's Hospital
Cleveland, Ohio, United States
Presenting Author(s)
Background: Rapid sequence intubation (RSI) in the pediatric emergency department (PED) is a low frequency procedure associated with a risk of adverse events. Timely post-intubation sedation is required to keep the intubated patient comfortable and unaware of the recent paralysis and intubation. Review of intubations at our institution revealed several areas for improvement during the RSI process. We therefore initiated a quality improvement (QI) project with a global aim to improve safety and minimize adverse events during RSI in the PED.
Objective: Our specific aim is to decrease the average time of post intubation sedative from a baseline of 20 minutes to 5 minutes over a 22-month period. The goal of 5 minutes was established based on expert consensus regarding the pharmacokinetics of rocuronium and etomidate, frequently used medications during RSI in our department.
Design/Methods: A multidisciplinary team convened to develop a key driver diagram (KDD) (Figure 1). Several interventions were undertaken during the study period using QI methodology with Plan Do Study Act (PDSA) cycles. These interventions included the development of an RSI checklist (Figure 2) and evidence-based clinical practice guideline, faculty education, simulation with front line staff, and a post-intubation survey. The primary outcome measure was the time to receiving post-intubation sedative. Process measures analyzed were checklist and video laryngoscope use. Our balancing measure was time in the trauma bay.
Results: Baseline data on intubation in the PED was collected over 18 months from between 2021 and 2022. PDSA cycles started in January 2023, following a pilot phase of checklist development and video laryngoscope training in 2022. Data was tracked using an I-MR chart. Special cause variation was noted in July 2023 after implementation of ongoing simulation with front line staff. The average time to post-intubation sedative administration had decreased from 20 minutes to 4 minutes, a decrease of 80% (Figure 3). Video laryngoscope use increased from 60% to 80% over the study period. The rate of checklist use is 50% since we began reliably measuring in March 2024. Data for our balancing measure of time in the trauma bay is under review.
Conclusion(s): This study demonstrates that our QI initiative was successful in achieving our goal of decreased time to post-intubation sedation, minimizing the risk for patients to be aware of their intubation. Continued evaluation of the process through data analysis is needed to demonstrate ongoing improvement and sustainability.
Figure 1
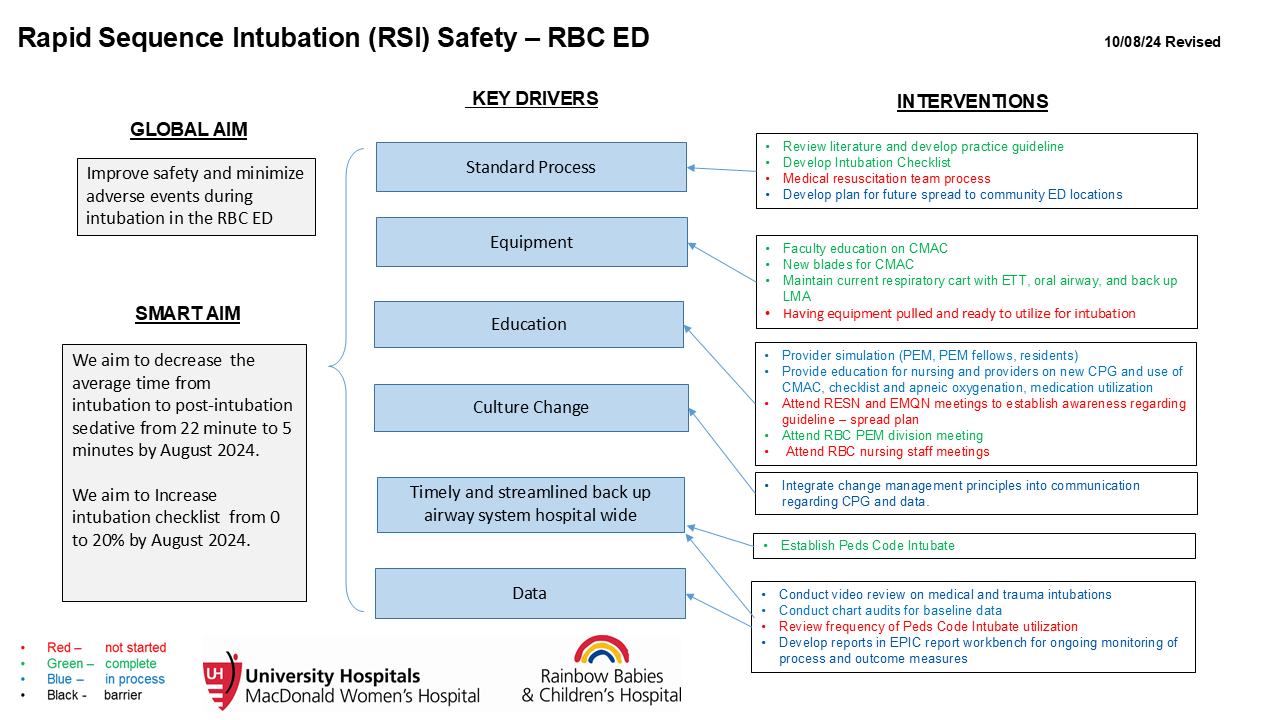 Key Driver Diagram
Key Driver DiagramFigure 2
.png) Front of our Intubation Checklist.
Front of our Intubation Checklist.Figure 3
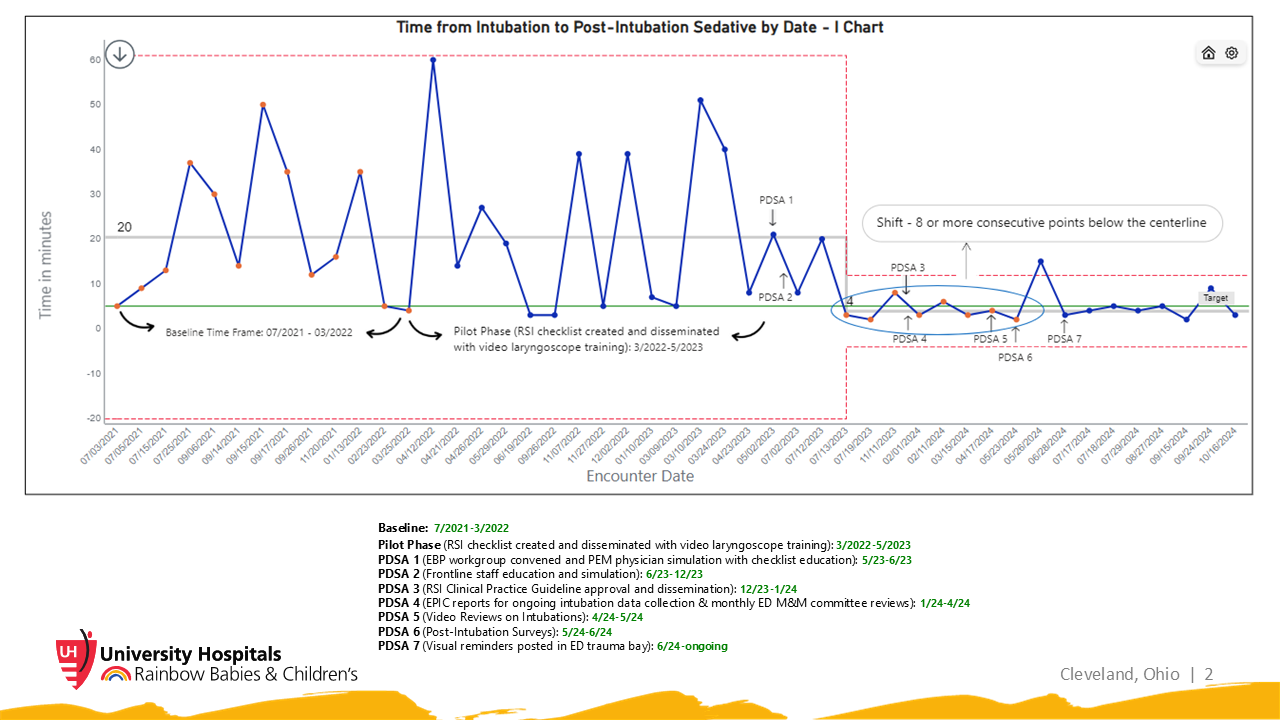 I-Chart with annotations detailing timeline of PDSA cycles. Special cause variation noted between PDSA cycles 3 and 4.
I-Chart with annotations detailing timeline of PDSA cycles. Special cause variation noted between PDSA cycles 3 and 4.

