Technology 2: Telemedicine
Session: Technology 2: Telemedicine
197 - The Impact of Targeted Workshops on Tele-Resuscitation Preparedness in Community Hospitals: The Oklahoma Experience
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 197.6798
Tavleen Sandhu, University of Texas Southwestern Medical School, Dallas, TX, United States; Lise DeShea, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Trassanee Chatmethakul, OUHSC, Oklahoma City, OK, United States; Morgan M. Grubb, OU Health, Norman, OK, United States; Jennifer Fang, Mayo Clinic, Rochester, MN, United States; Rachel A.. Umoren, University of Washington, Seattle, WA, United States; Abhishek Makkar, University of Texas Southwestern Medical School, Dallas, TX, United States
- TS
Tavleen Sandhu, MD (she/her/hers)
Assistant Professor of Pediatrics
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Approximately 50,000 neonates weighing < 1500 grams are born annually in the U.S., with 15-20% delivered in hospitals without a NICU. These infants, born in smaller community hospitals, face higher risks of adverse outcomes due to limited resources. Emergency situations can prevent maternal antenatal transfer to specialized centers, making immediate, high-quality neonatal care at community sites a crucial need. We hypothesized that neonatal tele-resuscitation training workshops can significantly enhance the skills and confidence of community hospital healthcare providers.
Objective: To assess the effectiveness of workshops in training community hospital providers in neonatal procedures and educating them on the use of tele-resuscitation service.
Design/Methods: In January 2023, Oklahoma Children’s Hospital launched a neonatal tele-resuscitation program offering resuscitation support to community hospital providers. This service targeted neonates born at 32 weeks or less, and those above 32 weeks requiring advanced resuscitation. Two inter-professional tele-resuscitation workshops were held for providers from community hospitals. The workshops included didactic sessions about the service, its clinical benefit, team communication strategies, and debriefing. Workshop attendees also practiced hands-on skills and participated in tele-resuscitation mock codes. Pre- and post-workshop surveys with Likert scale questions assessed the level of attendee confidence with advanced resuscitation procedures and the feasibility of the tele-resuscitation program in their practice. Changes in Likert ratings from pre- to post-workshop were analyzed using paired t-tests. Analysis was performed using R.
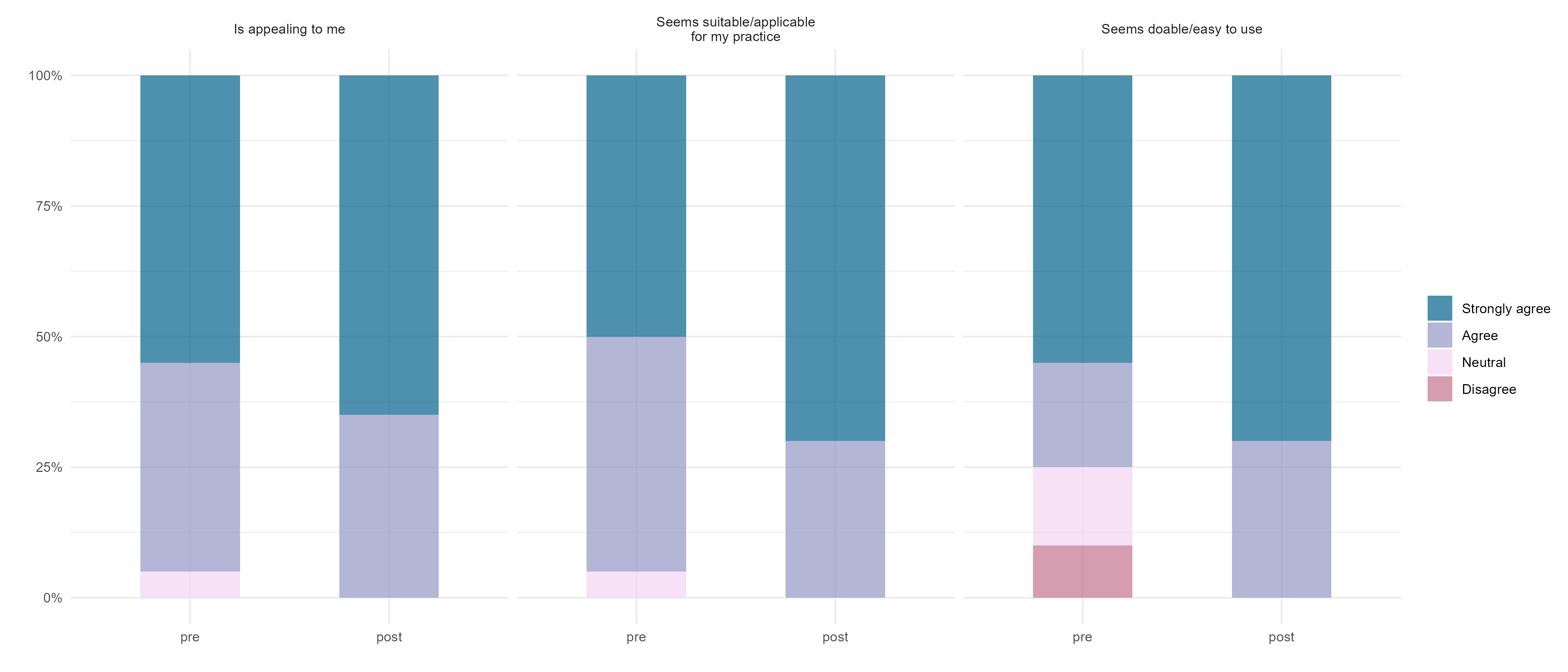
Results: Twenty providers attended the workshops from four community hospitals: five physicians (25%), 11 nurses (55%), and four respiratory therapists (20%). One-quarter of attendees reported prior experience with telemedicine and only one attendee, (5%) reported prior experience with tele-resuscitation. Participants demonstrated a significant increase in confidence from pre- to post-workshop in performing tasks such as intubation, umbilical line placement, needle thoracentesis, and debriefing, all p<.001 (Figure 1). Perceived feasibility of tele-resuscitation significantly improved after the workshop, p= 0.029 (Figure 2).
Conclusion(s): Neonatal tele-resuscitation workshops improved providers’ perceptions of the feasibility of such a program. Additionally, the skill sessions and mock codes increased their confidence with commonly performed procedures in an advanced neonatal resuscitation.
Figure 1. Provider confidence scores with neonatal procedures before and after the workshop

Figure 2. Provider impression of neonatal tele-resuscitation before and after the workshop