Medical Education 5: Procedures and Simulation
Session: Medical Education 5: Procedures and Simulation
242 - The Landscape of Procedural Skills in Neonatologists: Frequency, Comfort Levels, and Training Needs
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 242.6768
Beth Ann Johnson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Shelley Ehrlich, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Chunyan Liu, Cincinnati Children's Hospital, Cincinnati, OH, United States; Beena D. Kamath-Rayne, American Academy of Pediatrics, Itasca, IL, United States; Jennifer M. Brady, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Beth Ann Johnson, MD, MA, MEd
Neonatologist
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Clinical procedures are required – sometimes urgently – to care for sick neonates. There are no current data as to which procedures are routinely required of practicing neonatologists or the frequency thereof. It is also unknown how comfortable neonatologists are in performing procedures. Prior procedural studies in Pediatric Emergency Medicine report that critical procedures are rarely performed or required in clinical care and that most life-saving procedures occur too infrequently to maintain procedural skill.
Objective: This study seeks to broaden our understanding of procedural skill frequency and comfort over time for early, middle, and late career neonatologists.
Design/Methods: An online REDCap survey was distributed in 2021 through the American Academy of Pediatrics Section of Neonatal-Perinatal Medicine (SONPM) listserv. For this study, and in line with SONPM definitions, practicing neonatologists were divided into 3 groups based on years out of training: early-career ( < 7 years), mid-career (7 to 15 years), and late-career (>15 years).
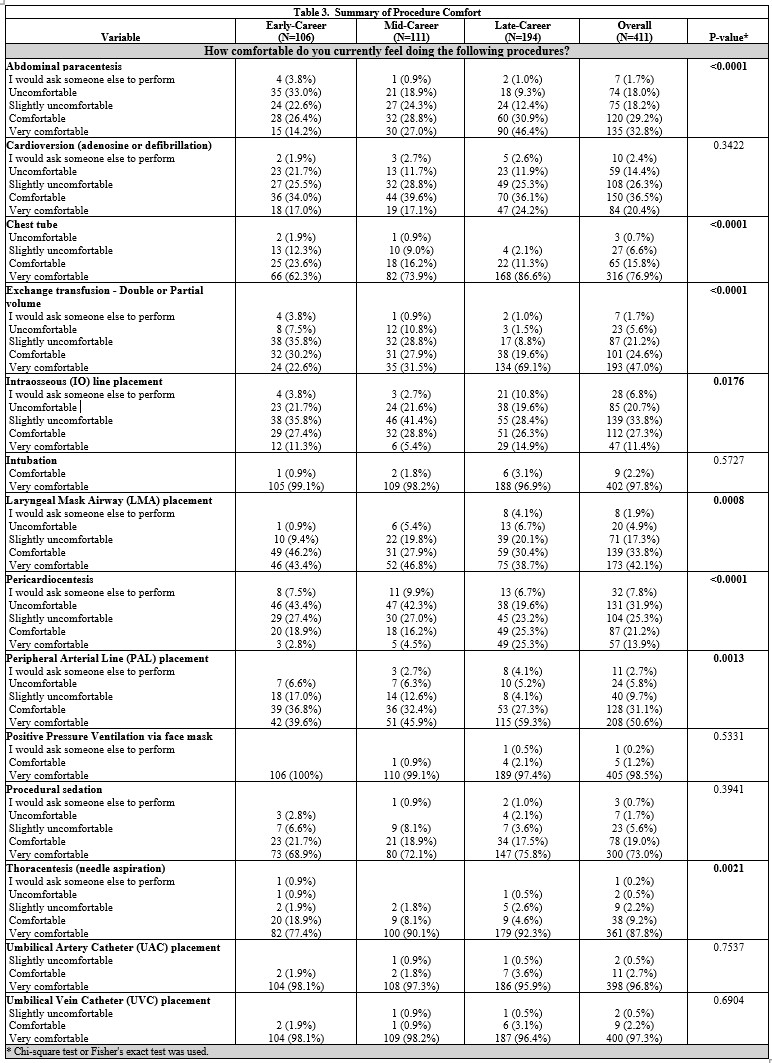
Results: 411 neonatologists completed the survey (Table 1). There was no difference in frequency of performing procedures amongst early, mid, and late career neonatologists (Table 2). Most procedures were performed less than 6 times in the last 12 months. Only two procedures, intubation and provision of positive pressure by facemask, were reported as performed > 5 times in the last year by >50% of respondents. The majority of neonatologists reported being comfortable or very comfortable performing most surveyed procedures (Table 3). For only 2 procedures, intraosseous line placement and pericardiocentesis, were more than 50% of respondents not comfortable. Pericardiocentesis was the only procedure where the majority (overall 51.8%) desired skill practice. Nearly half (45%) of respondents did not feel that direct patient care alone provided sufficient experience to maintain procedural skills.
Conclusion(s): Many critical procedures are performed infrequently by practicing neonatologists. Despite this fact, neonatologists across early, mid, and late career report being comfortable or very comfortable performing most procedures. Nearly half of responding neonatologists think clinical care is not enough to maintain skills, yet additional procedural practice is only desired by the minority. Even in busy units with high acuity, the overall rate of critical procedures may be too low to maintain clinical skills. By describing procedural exposure and comfort we can identify deficiencies, define practice needs, and create educational opportunities for faculty.
Table 1: Description of the study cohort
.jpg)
Table 2: Summary of procedure exposure
.jpg)
Table 3: Summary of procedure comfort