Technology 2: Telemedicine
Session: Technology 2: Telemedicine
195 - Telehealth Hammersmith Infant Neurologic Exam supports early diagnosis of cerebral palsy
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 195.6878
Jennifer C. Keene, University of Utah, Salt Lake City, UT, United States; Sarah Winter, University of Utah School of Medicine, Salt Lake City, UT, United States; Tara L. DuPont, University of Utah, Salt Lake City, UT, United States; Lauren Ayala, University of Utah School of Medicine, Salt Lake City, UT, United States; Wendy Evans, University of Utah School of Medicine, Salt Lake City, UT, United States; Betsy Ostrander, University of Utah School of Medicine, Salt Lake City, UT, United States

Jennifer C. Keene, MD, MS, MBA (she/her/hers)
Assistant professor of neonatal neurology
University of Utah
Salt Lake City, Utah, United States
Presenting Author(s)
Background: The Hammersmith Infant Neurologic Exam (HINE) is a validated, standardized assessment of the risk of cerebral palsy (CP) used to support early diagnosis of CP in the infantile period. The recent shift to telehealth has enabled more families to access high-risk neonatal follow-up clinics, but there is little work evaluating if the HINE can still be used in this setting.
Objective: This study aimed to compare the performance characteristics of telehealth vs in-person HINE examinations, and specifically to evaluate if telehealth HINE exams can be used to support early diagnosis of CP.
Design/Methods: This is a retrospective cohort study from a high-risk neonatal follow-up clinic with a multi-state catchment area which includes infants evaluated by either telehealth or in-person HINE by formally trained evaluators between 2018-2023. Fisher’s exact and Wilcoxon rank-sum tests were used to compare HINE scores at 3, 6, 9 and 12 months for patients with vs without CP in patients that were evaluated by telehealth or in-person.
Results: A total of 650 children (347 male) were included of which 244 (38%) had at least 1 telehealth HINE and 148 (23%) were diagnosed with CP with median age at last follow-up of 24 months. HINE was associated with CP at 3,6,9 and 12-months for both telehealth and in-person exams (telehealth p= 0.01 to < 0.0001; sensitivity 50-100% and specificity 69-93%, in-person p< 0.0001; sensitivity 69-83% and specificity 88-97%) (Table 1, Figure 1). The HINE scores which optimally differentiated those with and without CP at 3,6,9 and 12 months in-person were 45, 52, 63 and 63 and via telehealth were 55,54,64 and 60. There was no significant difference in area under the receiver operating curve between in-person and telehealth evaluations at any age (Table 2).
Conclusion(s): Telehealth and in-person HINE evaluation across the first year of life were both highly effective for supporting early CP diagnosis. Extending the use of HINE testing to telehealth provides an opportunity to increase early diagnosis of CP in settings with limited resources and long geographic distances to specialty NICU follow-up clinics. Further work is needed to improve access to developmental testing to all infants with a high risk for neurodevelopmental delay.
Table 1
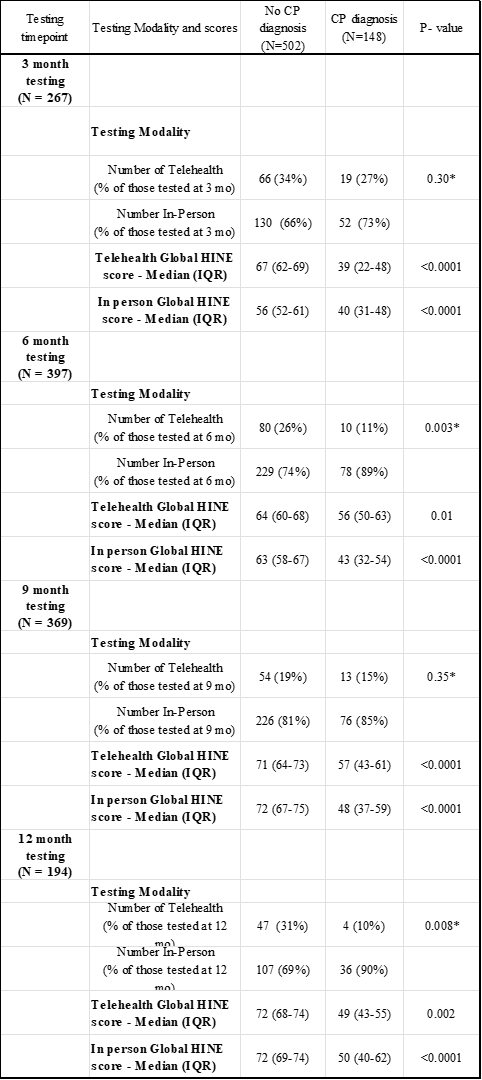 CP - Cerebral Palsy, HINE - Hammersmith Infant Neurologic Exam, IQR - Interquartile range (25%ile - 75%ile), * p-value calculated for overall Fisher's exact comparison between patients who do and do not have CP
CP - Cerebral Palsy, HINE - Hammersmith Infant Neurologic Exam, IQR - Interquartile range (25%ile - 75%ile), * p-value calculated for overall Fisher's exact comparison between patients who do and do not have CPFigure 1
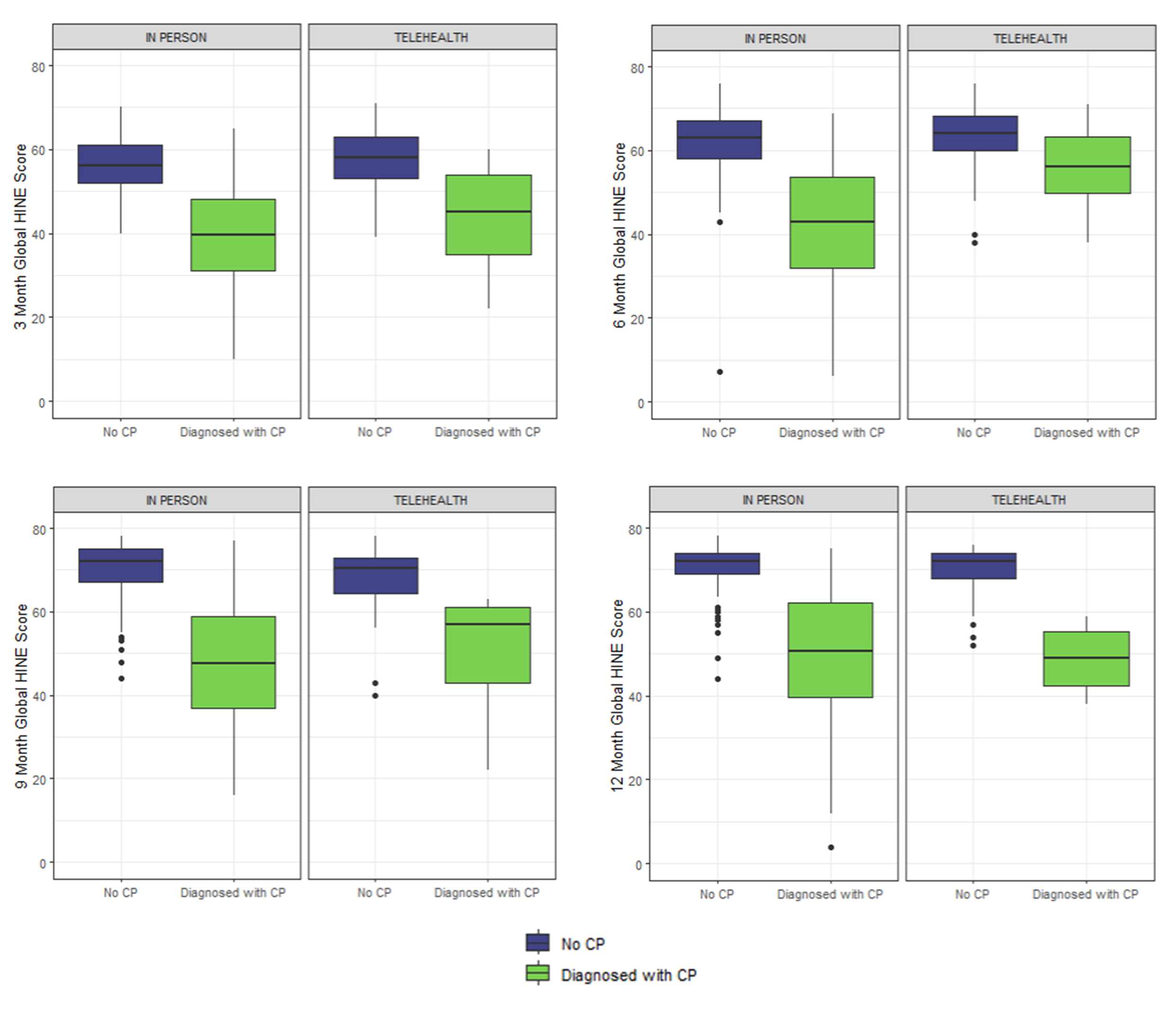 Comparison of Global Hammersmith Infant Neurologic Exam (HINE) scores at 3, 6, 9 and 12 months for patients with vs without CP for visits that were conducted either in-person or via telehealth exam. Global HINE scores were significantly different for patients with and without CP at all time timepoints and by both exam modalities
Comparison of Global Hammersmith Infant Neurologic Exam (HINE) scores at 3, 6, 9 and 12 months for patients with vs without CP for visits that were conducted either in-person or via telehealth exam. Global HINE scores were significantly different for patients with and without CP at all time timepoints and by both exam modalitiesTable 2
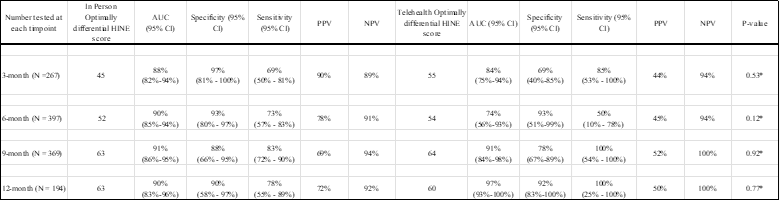 AUC = Area Under Curve, CI - Confidence Interval, HINE - Hammersmith Infant Neurologic Exam, IQR - Interquartile range (25%ile - 75%ile), NPV = Negative predictive value, PPV = Positive predictive value, * p-value calculated for the comparison of AUC between Telehealth and In-Person HINE exams
AUC = Area Under Curve, CI - Confidence Interval, HINE - Hammersmith Infant Neurologic Exam, IQR - Interquartile range (25%ile - 75%ile), NPV = Negative predictive value, PPV = Positive predictive value, * p-value calculated for the comparison of AUC between Telehealth and In-Person HINE exams
