Neonatal Quality Improvement 4
Session: Neonatal Quality Improvement 4
511 - Using Equity Focused Quality Improvement to Reduce Breastmilk Disparities for Preterm Infants in a Single-Center Intensive Care Nursery
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 511.6613
Lucky Ding, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Kayla Karvonen, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Jeannie Chan, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Michele Evans, UCSF Benioff Children's Hospital San Francisco, Martinez, CA, United States; Courtney Gregory, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Maria Hetherton, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Susan McLaughlin, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Diana Rogosa, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Katelin Kramer, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States
- LD
Lucky Ding, MD (she/her/hers)
Pediatrics Resident PGY-3
UCSF Benioff Children's Hospital San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: Maternal breastmilk (MBM) has many health benefits for preterm infants. Racial and ethnic disparities in MBM provision at discharge (DC) from the NICU have been shown nationally and locally in our Intensive Care Nursery (ICN); 46% of Black and Latinx preterm infants receiving majority MBM at DC or transfer compared to 65% of Non-Hispanic White and Asian infants.
Objective: This equity focused quality improvement (EFQI) project aims to increase the rate of Black/Latinx preterm infants ( < 34 weeks gestational age) receiving majority MBM at DC/transfer by 30% (from 45% to >60%) over 3 years (by Jan 2027).
Design/Methods: This EFQI initiative was performed at an academic level IV NICU. A multi-disciplinary team met twice monthly during the planning stage, including a parent survey of breastfeeding challenges. Using core quality improvement (QI) methodology, a key driver diagram was created to develop targeted interventions. Interventions included an in-house California WIC (Women, Infants, and Children) loaner pump program, unit-wide screening for hospital grade pump access, antepartum lactation consultations, lactation tip sheets, and introduction of culturally responsive community-based lactation and peer support groups. Interventions are ongoing. The primary outcome is the rate of MBM at DC/transfer by race and ethnicity. Process measures include adherence to interventions above. Data is collected from monthly chart review and analyzed with run charts and t-tests.
Results: The pre-intervention period was from Jan-Apr and Nov-Dec 2023 (N=46) and the initial post-intervention period was from Jan-Jul 2024 (N=44). There has been improvement in the outcomes, with an increase in the rate of Black/Hispanic preterm infants receiving majority MBM at DC from 46% to 67% (p=0.17) and 100% MBM at DC from 21% to 48% (p=0.06). Overall rates of preterm infants receiving majority MBM at DC has also improved from 52% to 70% (p=0.08) and 100% MBM at DC from 28% to 55% (p=0.01). Improvement was associated with adherence to the process measures, with 100% of mothers screened for hospital grade pump access and 59% of eligible mothers receiving a loaner WIC pump.
Conclusion(s): Using core EFQI methodology, we successfully launched targeted, multi-disciplinary interventions to reduce racial and ethnic inequities in MBM provision rates in preterm infants. Initial data shows an associated increase in MBM provision at DC for Black/Hispanic preterm infants. Next steps include continued implementation of targeted interventions and ongoing data collection.
Figure 1. Key Driver Diagram
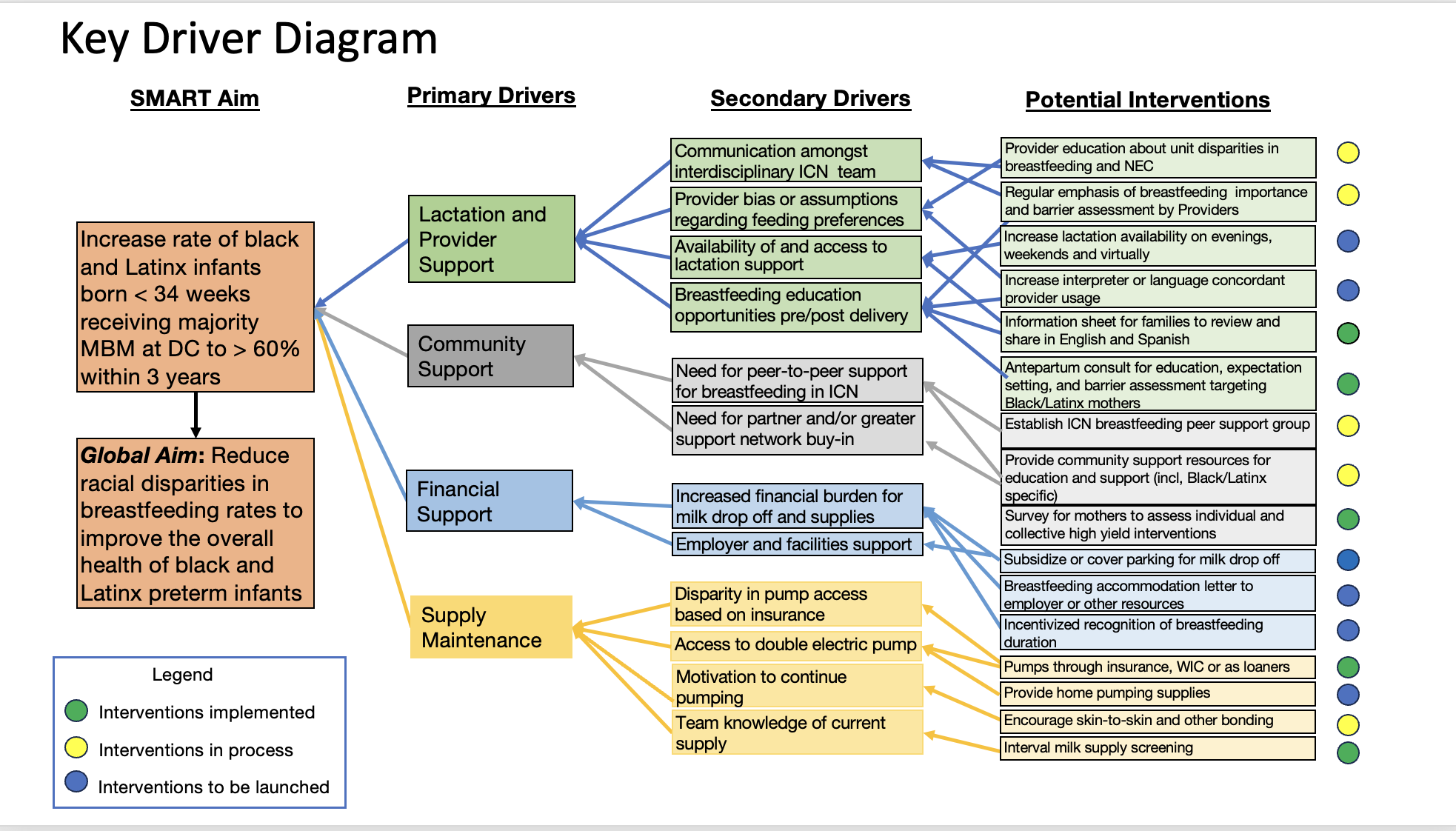
Figure 2. Outcomes and Process Metrics
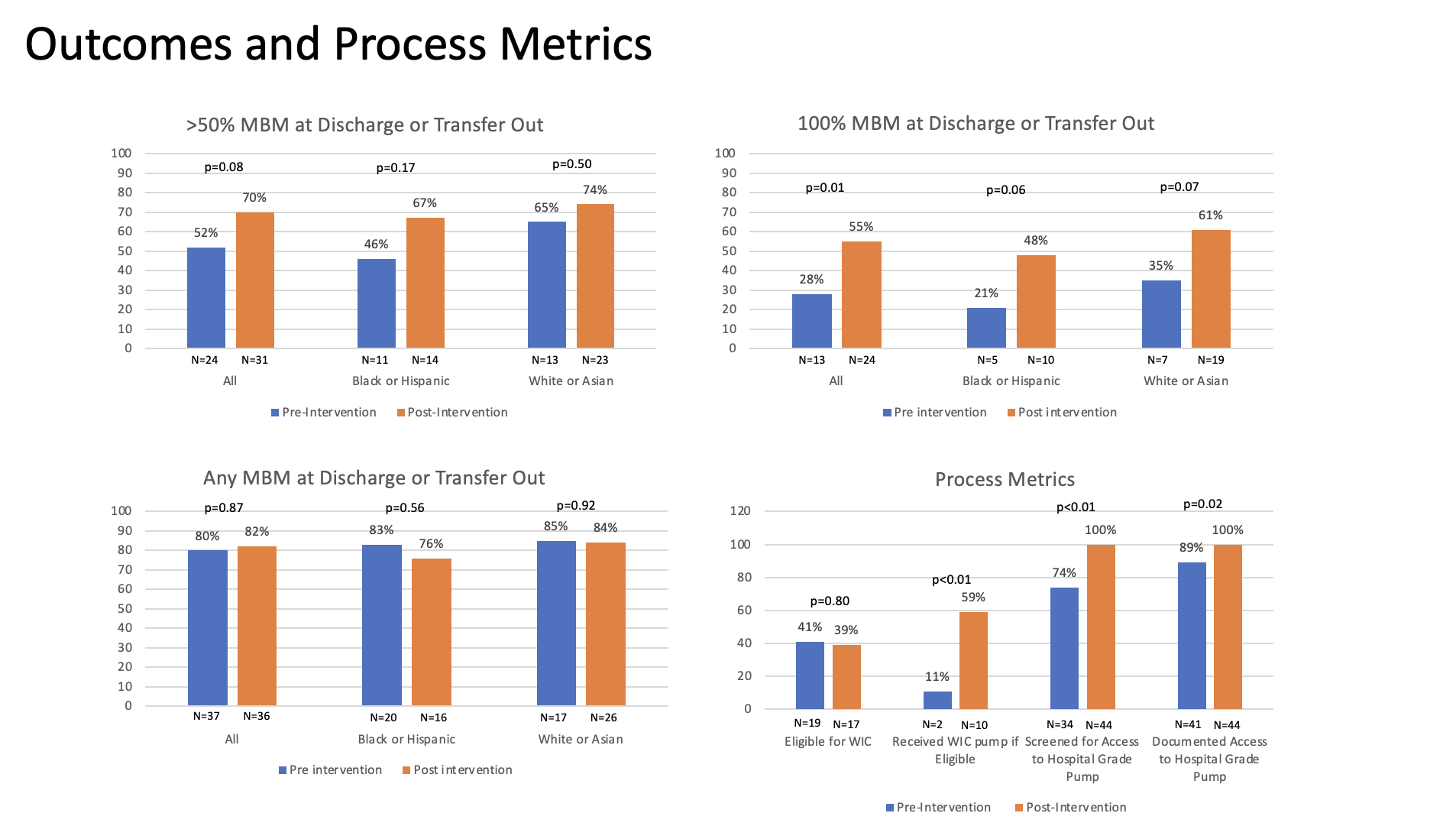
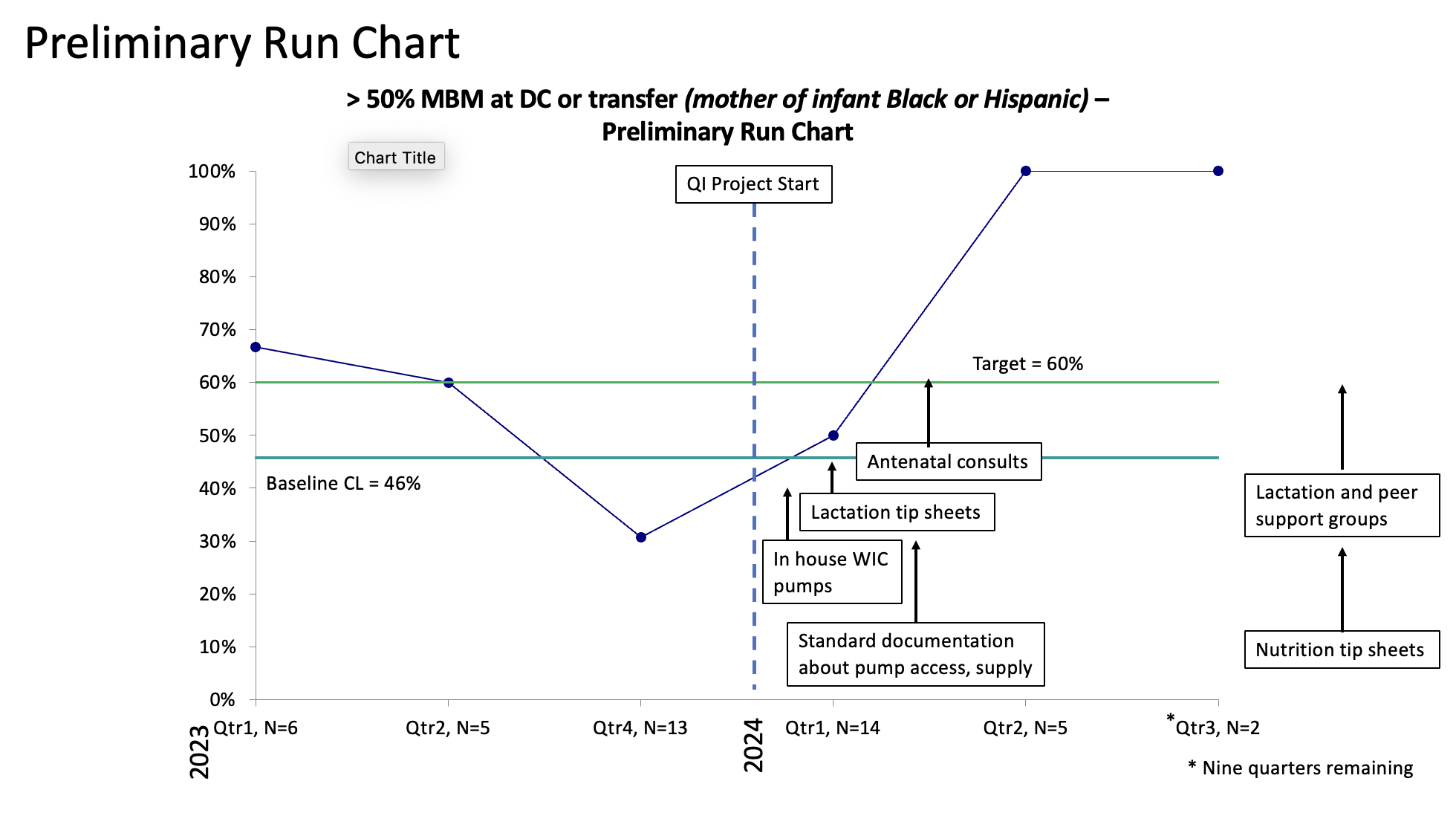
Figure 3. Preliminary Run Chart
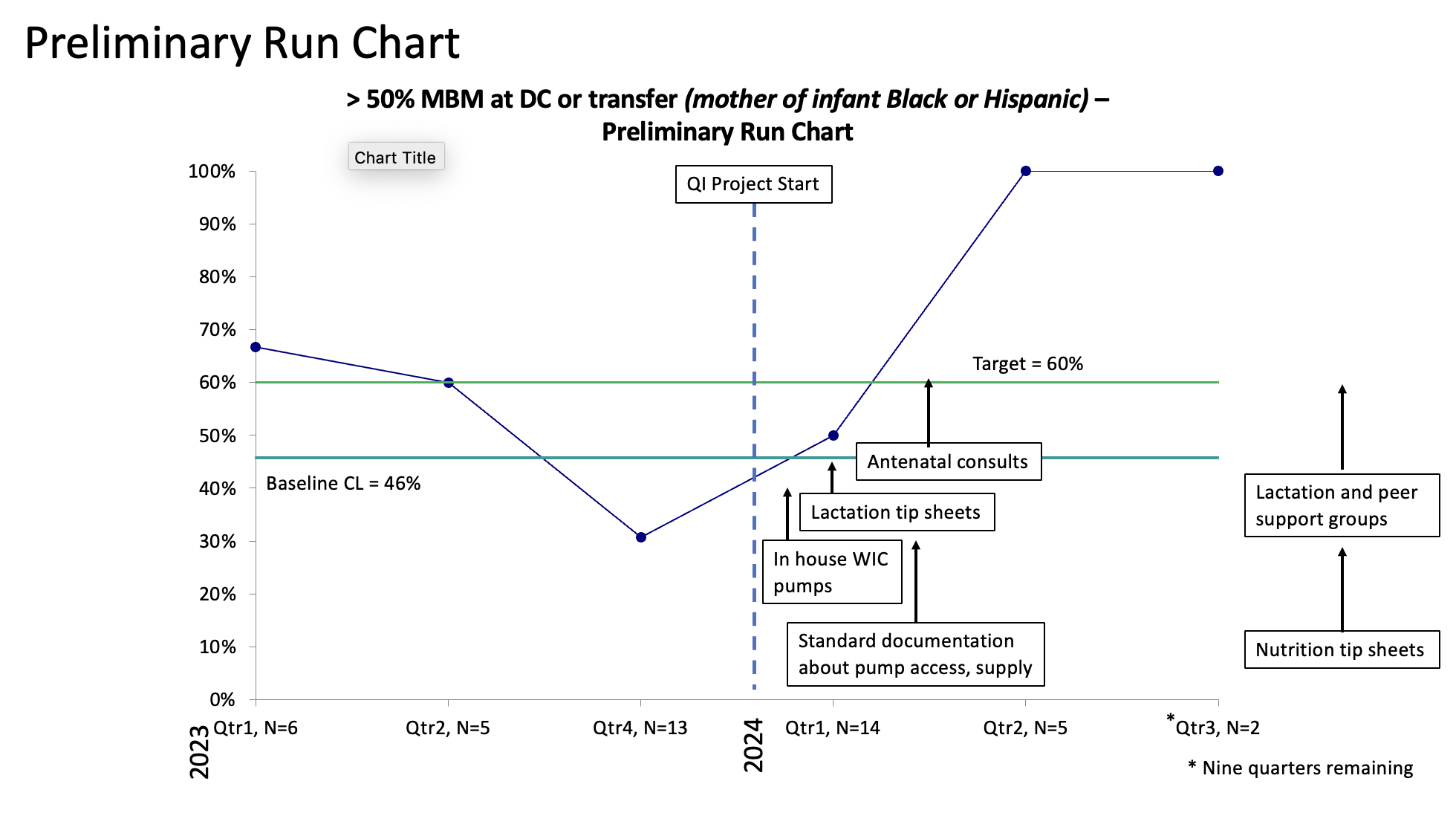
Figure 1. Key Driver Diagram
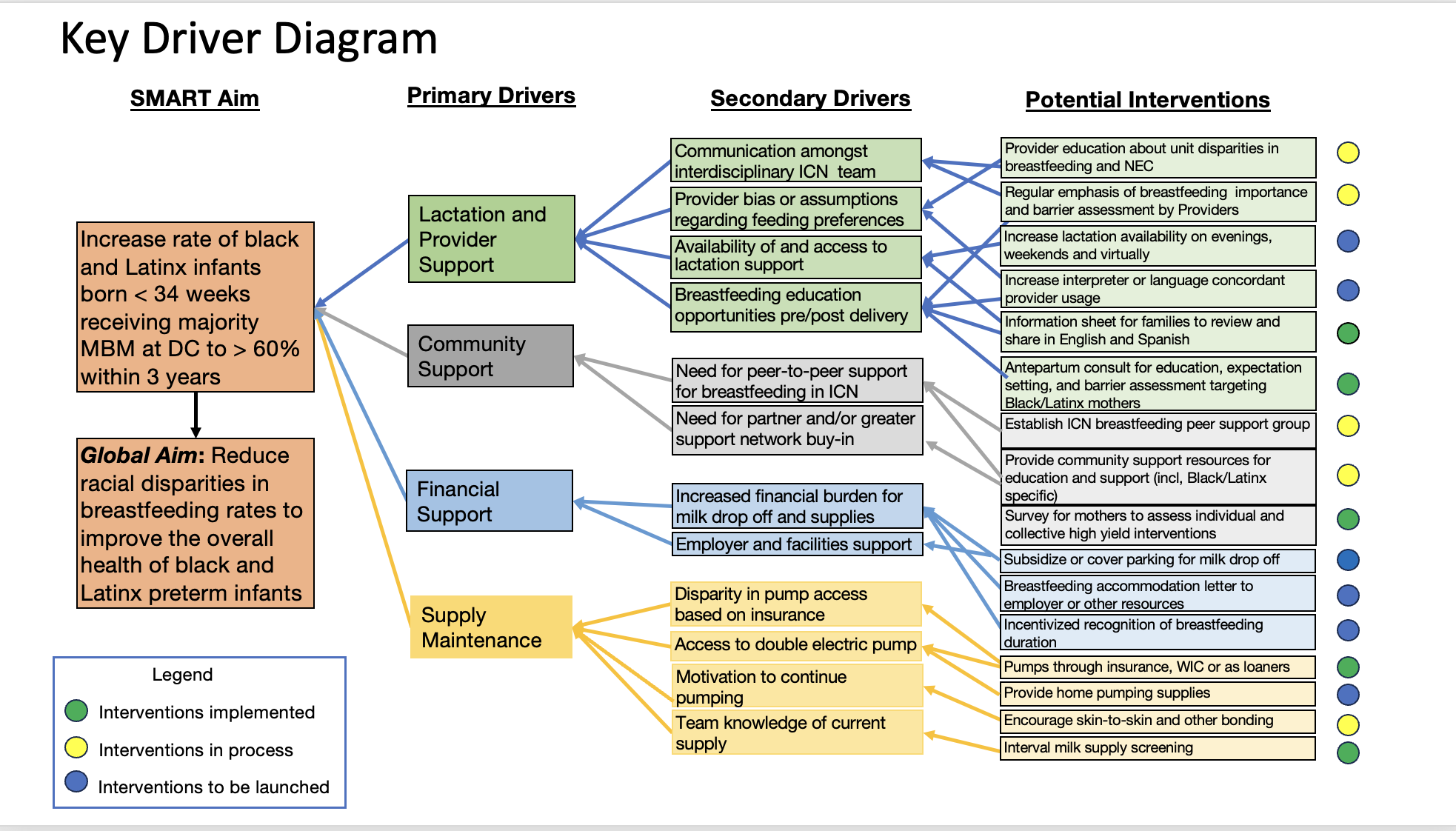
Figure 2. Outcomes and Process Metrics
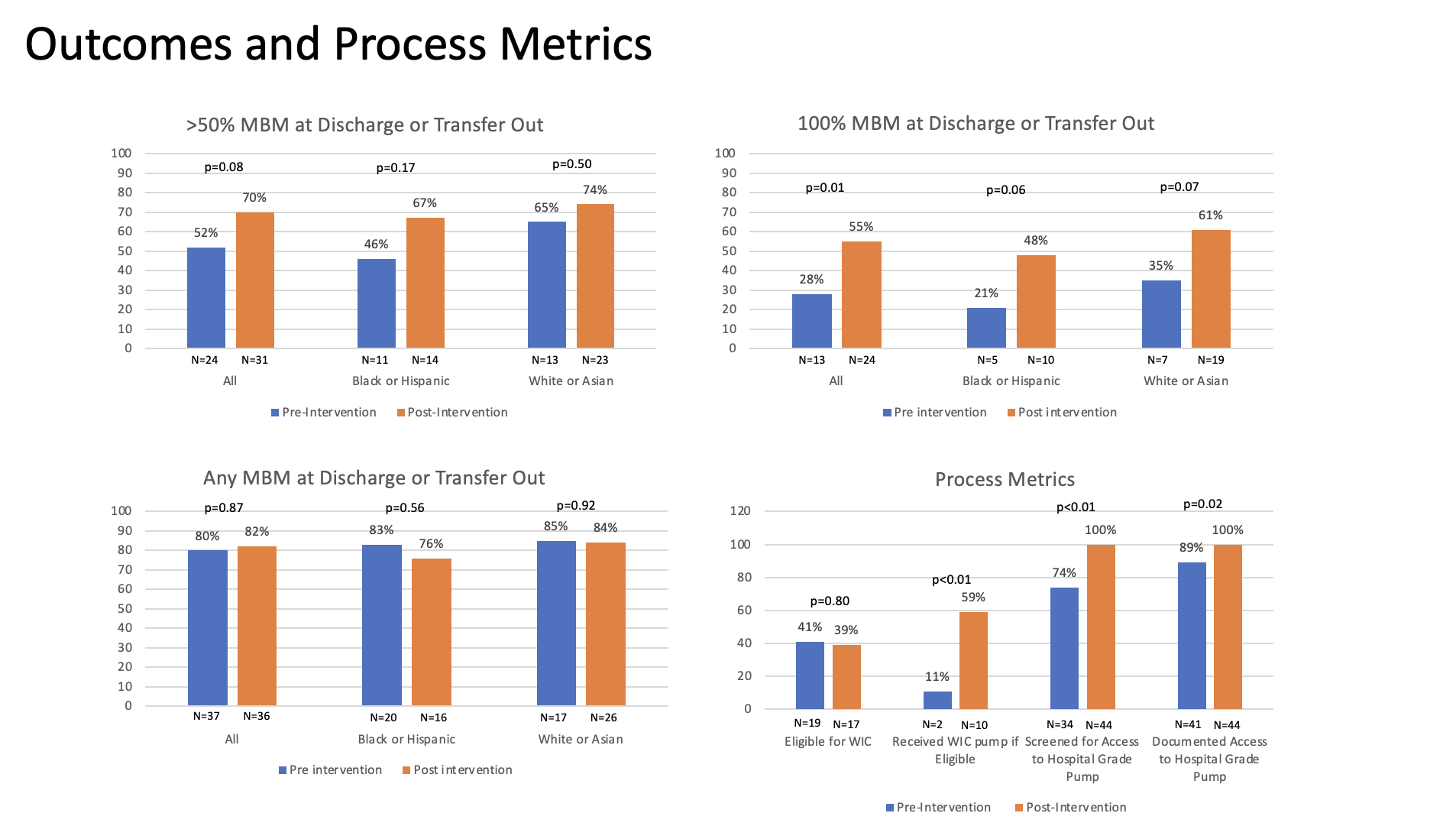
Figure 3. Preliminary Run Chart