Emergency Medicine 4
Session: Emergency Medicine 4
254 - Routine HIV Screening in a Urban Pediatric Emergency Department
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 254.6454
Jessica Schmitt, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Rachel Danzig, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Michael Arnold, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Alton Dueks, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Julia Rosebush, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Moira McNulty, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Kimberly Stanford, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States
- JS
Jessica Schmitt, LCSW (she/her/hers)
Director, HIV Clinical Engagement
University of Chicago Division of the Biological Sciences The Pritzker School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background: Adolescents and young adults ages 13-24 (AYA) are a highly vulnerable population to HIV, making up nearly 20% of new HIV diagnoses in the US in 2022. Although routine HIV screening is recommended for adolescents by the American Academy of Pediatrics, Centers for Disease Control and Prevention (CDC), and U.S. Preventive Services Task Force, integration of HIV screening and prevention efforts into US pediatric emergency departments (PEDs) has been slow.
Objective: University of Chicago Medicine (UCM) has provided routine opt-out HIV screening in the adult emergency department for everyone between ages of 18-64 since 2016. In July 2022, to align with CDC guidelines and improve rates of HIV screening among AYA, UCM’s PED created an adapted routine HIV screening program in which a best practice alert (BPA) was added to the electronic medical record (EMR) to prompt routine HIV screening for adolescents being tested for gonorrhea/chlamydia or receiving a blood draw. HIV screening rates and detection of new HIV diagnoses in the PED following implementation of these BPAs was assessed.
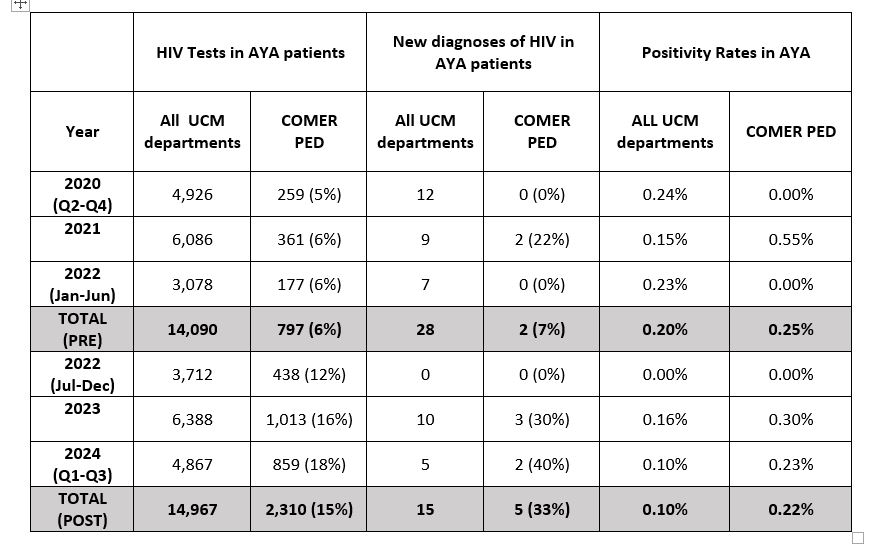
Design/Methods: We conducted a retrospective review of HIV screening rates and new HIV diagnoses among AYA from March 1, 2020, to September 30, 2024. We examined HIV screening volumes, new diagnoses, positivity rates, and linkage to care during the 27-month period before and after the implementation of PED routine HIV screening . The proportion of HIV tests and new HIV diagnoses in the UCM PED was compared to the total tests and diagnoses across all departments, both pre- and post-implementation.
Results: HIV tests performed in UCM PED increased 189% and identification of new HIV diagnoses increased 150% following the implementation of BPA alerts. The proportion of positive HIV tests from UCM PED increased from 6% to 15% post implementation, as well as UCM PED identifying a higher proportion of new diagnoses (7% vs. 33%). Positivity rates were higher in PED than all UCM department for all months. There were no changes in linkage to care as all new AYA diagnoses from UCM PED were linked to care.
Conclusion(s): Implementation of routine HIV screening allowed UCM PED to identify more new HIV diagnoses among AYA, in line with previous reports. Similar to adult populations, more HIV diagnoses were identified through the PED compared to other hospital settings. Although there are barriers to implementation in an AYA population, routine HIV screening in PEDs is feasible and provides an important opportunity for early identification of new HIV diagnoses and linkage to care, as well as provide education and de-stigmatization of HIV.
HIV Screening and New HIV Diagnoses