Emergency Medicine 6
Session: Emergency Medicine 6
287 - Reducing Antibiotic Overuse in Immunocompetent Children with Febrile Neutropenia in a Pediatric Emergency Department: A Quality Improvement Initiative
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 287.6464
Katherine Girgulis, University of Calgary, Calgary, AB, Canada; Jennifer Thull-Freedman, University of Calgary, Calgary, AB, Canada; Nicola AM. Wright, University of Calgary, Calgary, AB, Canada
- JT
Jennifer Thull-Freedman, MD, MSc
Clinical Professor
University of Calgary
Calgary, Alberta, Canada
Presenting Author(s)
Background: Management of febrile neutropenia in previously healthy, presumed immunocompetent children varies. Overtreatment burdens patients, families, and the healthcare system. With guidance from a new Canadian Paediatric Society (CPS) Practice Point, most well-appearing children can be managed without antibiotics or hospital admission.
Objective: Our aim was to safely reduce nonindicated antibiotic use from 7% to under 5% within one year of the July 2023 Practice Point publication.
Design/Methods: A multidisciplinary team planned reviewed all charts of febrile ED patients found to be neutropenic. Exclusion criteria mirrored the CPS Practice Point. Antibiotics were classified as indicated or non-indicated according to CPS Practice Point definitions. Records from the preceding year were reviewed retrospectively to assess baseline performance. Interventions included guideline dissemination, provider education, creation of an app-based reference, and sharing of EMR smart phrases. The primary outcome was proportion of children receiving nonindicated antibiotics. Additional outcomes included hospital admission, overall proportion of children receiving antibiotics, and completion of appropriate laboratory follow-up. Rates of ED revisits and missed serious bacterial infections were assessed as balancing measures. Outcomes were evaluated descriptively and with statistical process control (SPC) charts. Because of the low baseline occurrence of the primary outcome, an SPC G chart was used to detect special cause variation. Primary care providers were contacted when recommended laboratory follow-up did not occur and were asked to provide feedback regarding barriers.
Results: Three hundred and ninety-eight (398) children were included. The proportion of non-indicated antibiotics was 6.7% at baseline. Following tests of change, special cause variation was demonstrated with 97 consecutive cases occurring without error (non-indicated antibiotics). Following the occurrence of special cause variation until the end of the study, only 1.6% of children received non-indicated antibiotics. There was no increase in re-presentations to ED (9% vs 8%; p=0.65) nor missed SBI (0% vs 0%). Influenza was prevalent during the intervention period, accounting for 71% of positive viral tests (n=64/90).
Conclusion(s): QI methodology successfully facilitated the timely adoption of best practices to align local clinical care with national guidelines. Low-risk children with febrile neutropenia were able to safely avoid unnecessary antibiotic exposure, demonstrating an opportunity to reduce low-value treatment while enhancing patient-centered care.
Table 1
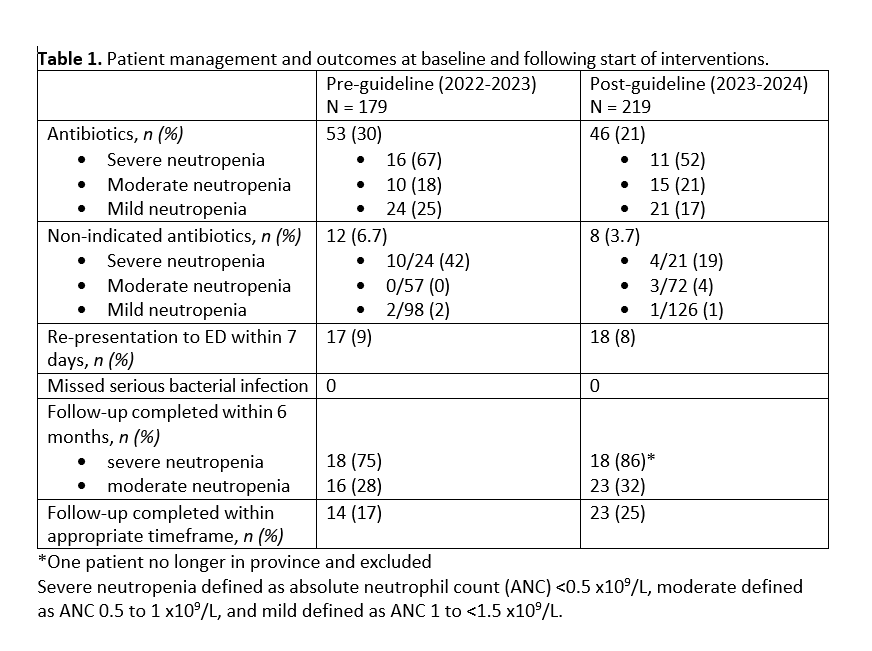 Management of ED patients with febrile neutropenia before and after the start of interventions
Management of ED patients with febrile neutropenia before and after the start of interventionsFigure 1: Use of non-indicated antibiotics in ED patients with febrile neutropenia
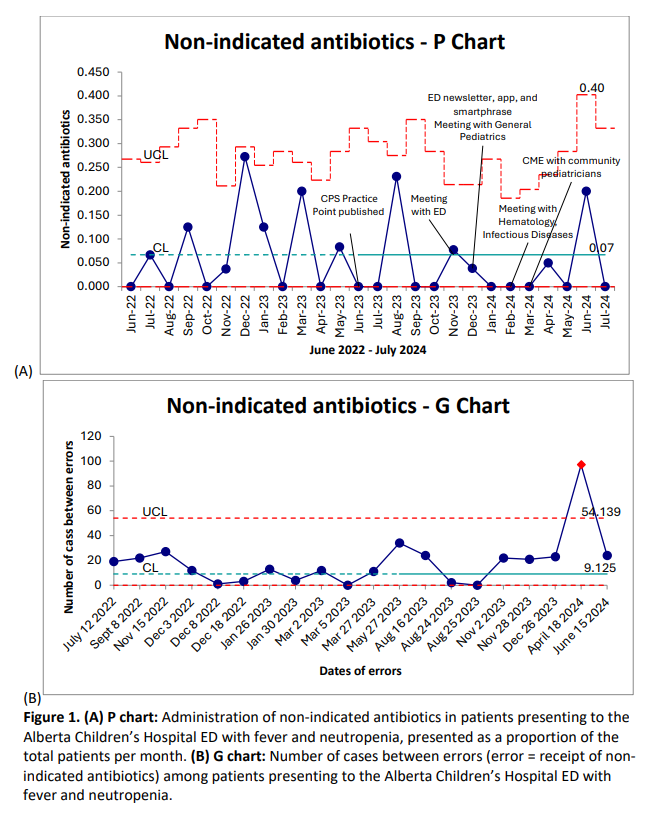 P-chart and G-chart for primary outcome of proportion of otherwise well children with febrile neutropenia receiving non-indicated antibiotics in the ED. G-chart demonstrated number of cases appropriately treated between occurrences of inappropriate treatment.
P-chart and G-chart for primary outcome of proportion of otherwise well children with febrile neutropenia receiving non-indicated antibiotics in the ED. G-chart demonstrated number of cases appropriately treated between occurrences of inappropriate treatment. 

