Neonatal Quality Improvement 5
Session: Neonatal Quality Improvement 5
522 - Quality Initiative to Reduce NICU Admissions for Hypoglycemia: Comparison of Previous and Revised Hypoglycemia Management Guidelines at Women & Infants Hospital (WIHRI)
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 522.6523
Dolapo S. AVUNGBETO, Women & Infants Hospital of Rhode Island, DOWNINGTOWN, PA, United States; Nkechi E. okotcha, Nkechi Okotcha, JOHNSTOWN, PA, United States; Avery Zierk, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Abbot Laptook, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Nicholas GG. Guerina, Women & Infants Hospital of Rhode Island, Providence, RI, United States
- DA
Dolapo S. AVUNGBETO, MD (he/him/his)
Attending
Women & Infants Hospital of Rhode Island
DOWNINGTOWN, Pennsylvania, United States
Presenting Author(s)
Background: Babies born ≥35 weeks gestation at risk for hypoglycemia are managed with blood glucose monitoring and treatment of hypoglycemic events with continued feeding plus oral glucose gel. Guideline triggers for NICU (possible need for IV dextrose) include a critical low blood glucose, or failure to achieve euglycemia after receiving a specified number of consecutive, or total number of gel doses. At WIHRI the guideline in use in 2021 resulted in 20-30% of hypoglycemic babies eventually meeting criteria for transfer to the NICU, but 70% of those admitted did not require IV dextrose. The WIHRI NICU Quality Committee conducted a multidisciplinary review process to redesign the guideline with a goal of safely reducing NICU admissions (Table 1).
Objective: The primary outcome tracked the percent of hypoglycemic babies requiring NICU admission with the new compared to the old hypoglycemia management guidelines.
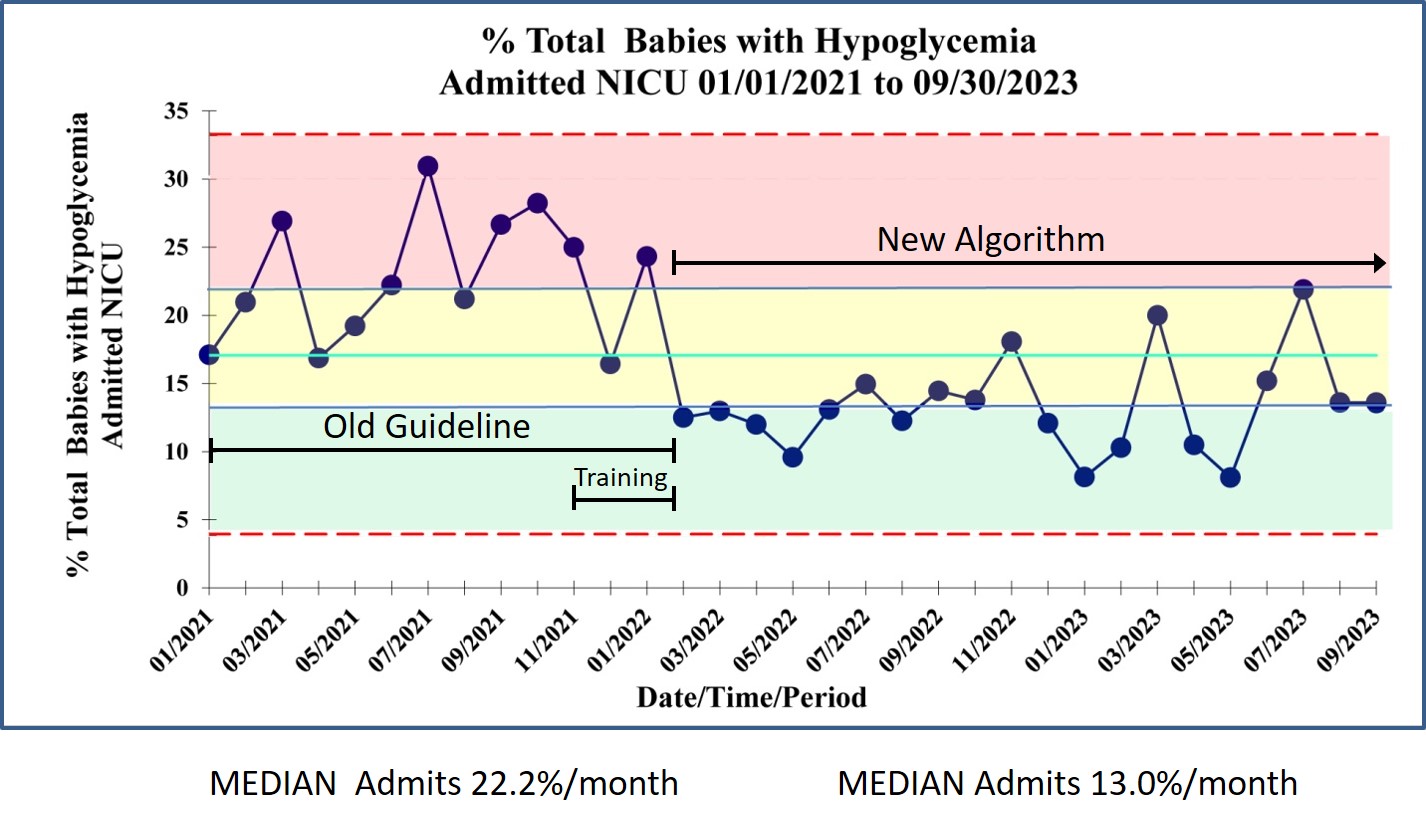
Design/Methods: Retrospective EMR reviews were conducted from 01/01/2021 through 09/30/2023, and included data for 10 months under the old guideline and 20 months after rollout of the new guideline. All babies undergoing routine newborn care requiring management for hypoglycemia were identified, and those babies requiring NICU admission underwent additional birthing person and newborn EMR data abstraction. Data collection
included demographics, antenatal and intrapartum conditions, mode of delivery, risk factors for hypoglycemia, IV dextrose use, length of hospital stay (LOS), and threshold triggers for NICU admission. Data were analyzed by descriptive statistics and the primary outcome was tracked with a statistical process control chart (Figure 1).
Results: There were no statistically significant differences between guidelines in birthing person age or ethnicity, incidence of hypertension/preeclampsia, diabetes, or use of betablockers, delivery mode, average birthweight, gestational age, occurrence of IUGR/SGA, 5 min APGAR <7, or cord pH <7.2. There was a significant reduction in the percent NICU admissions between the old and new guideline from a median of 22.2% (199/854) to 13.1% (219/1659), respectively (p=0.0001) (Table 2). For both guidelines, the main trigger for NICU admission was threshold glucose values. The proportion of babies requiring IV glucose remained relatively low with both guidelines (31.1% versus 35.2%). There was no significant difference in overall LOS (4.0 ± 3.7 versus 4.3 ± 5.5 days).
Conclusion(s): The new hypoglycemia guideline significantly reduced the need for babies to be separated from their mother for NICU care.
Dolapo Avungbeto CV
Dolapo Avungbeto CV 2023 pdf pas.pdf
Table 2 - Comparison of outcome measures old vs new guideline.
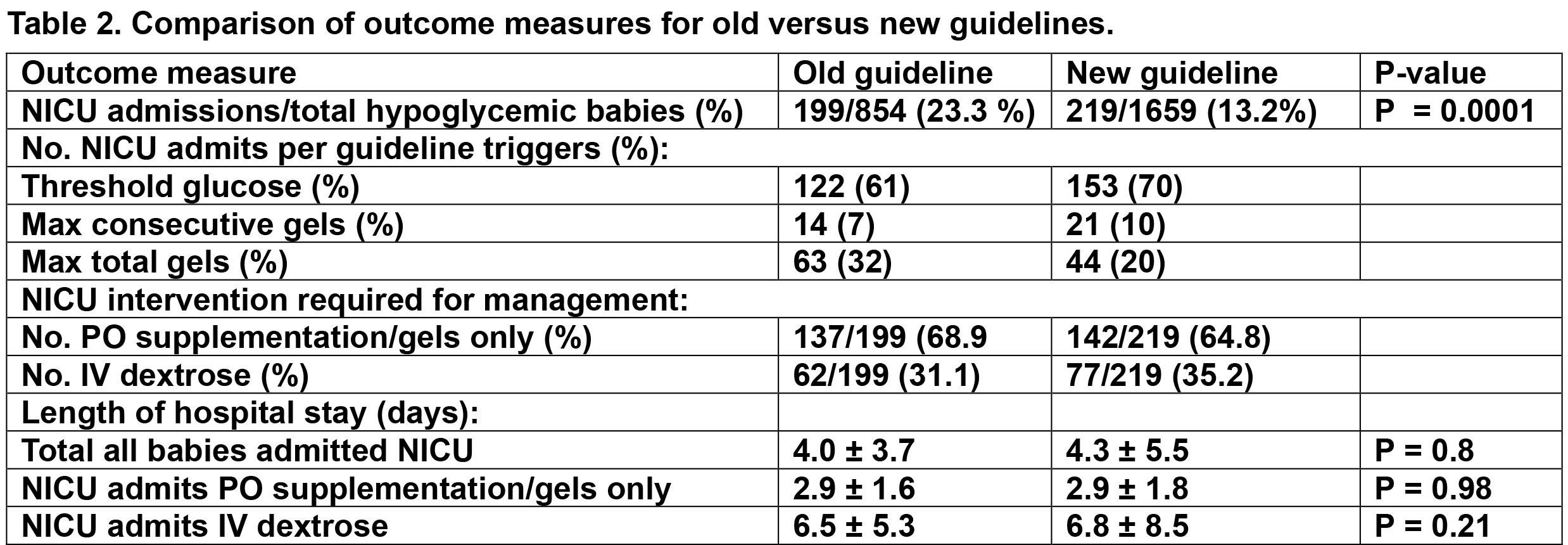
Figure 1 - Control chart Percent NICU admissions per month