Emergency Medicine 5
Session: Emergency Medicine 5
271 - The Butterfly BVM, a Novel Resuscitator in Pediatric Resuscitation
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 271.6536
Mariju Baluyot, Riley Hospital for Children at Indiana University Health, Fishers, IN, United States; Jackson Hamersly, Indiana University School of Medicine, Carmel, IN, United States; Ryan Stambro, Indiana University Health, In, IN, United States; Rachell J. Laughlin, Indiana University School of Medicine, Indianapolis, IN, United States; Benjamin Nti, Indiana University School of Medicine, Carmel, IN, United States

Mariju Baluyot, MD (she/her/hers)
Assistant Professor of Clinical Emergency Medicine and Pediatrics
Riley Hospital for Children at Indiana University Health
Fishers, Indiana, United States
Presenting Author(s)
Background: Bag-valve-mask (BVM) resuscitators, like the Ambu-bag, are commonly used to ventilate patients in respiratory failure but are often misused, even by trained personnel, leading to volutrauma or barotrauma. Traditional BVMs provide no adequate means of restricting the volume of air delivered (tidal volume) or peak inspiratory pressure (PIP) when the bag is squeezed. This risk is heightened in pediatrics, where lung volumes vary with age. The Butterfly BVM resuscitator was developed to address these issues, incorporating volume and pressure control to help regulate safer ventilation.
Objective: The primary objective of this study was to compare minute ventilation (MV) of the Butterfly BVM to a traditional BVM (Ambu-bag) in simulated resuscitations irrespective of participant administering the device.
Design/Methods: This was a prospective research study testing the Butterfly BVM and the Ambu Bag on infant- and adolescent-sized mannequins during simulated resuscitations. Resuscitation was administered by three groups (physicians, nurses, and emergency medical technicians [EMT]). Tidal volume was measured with an ASL 5000 device, and respiratory rate was counted manually via recordings of each simulation session. These values were used to calculate MV delivered by each participant during the simulation.
After several minutes of bagging during sessions, participants were asked to optimize pressure delivered during bagging with either a pressure manometer attachment on the Ambu-bag, or by maximizing pressure delivered without changing PIP settings on the Butterfly BVM.
Results: Twenty-one simulations were conducted with 42 participants (21 physicians, 10 nurses, and 11 EMTs). There was improvement in MV delivery after PIP optimization for 21.4% (9/42) resuscitations using the Butterfly BVM compared to 4.7% (2/42) resuscitations using the Ambu-bag. Additionally, there was worsened MV delivery after PIP optimization for 7.1% (3/42) of resuscitations using the Butterfly BVM compared to 21.4% (9/42) of resuscitations utilizing the Ambu-bag. Refer to Table 1 for full data.
Participants overall showed an increase in adequate MV delivery with the Butterfly BVM both before and after PIP optimization, and even if there was inadequate resuscitation delivered with the Ambu-bag. Please see Table 2a and Table 2b for full data.
Conclusion(s): The Butterfly BVM resuscitator demonstrated more consistent control over minute ventilation compared to the traditional Ambu-bag in simulated pediatric and adult resuscitations, suggesting its potential to enhance safe and effective ventilation across various provider groups.
Table 1
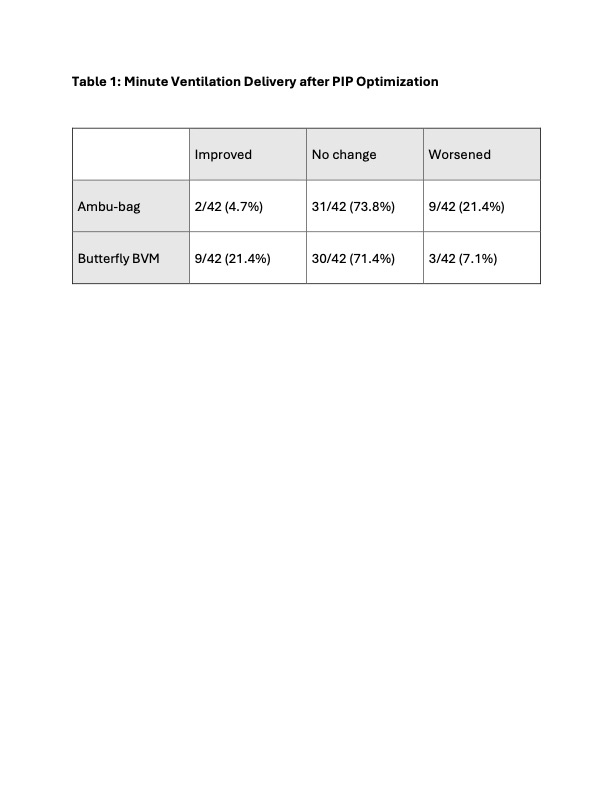 Table 1: Minute Ventilation Delivery after PIP Optimization
Table 1: Minute Ventilation Delivery after PIP Optimization Table 2a and Table 2b
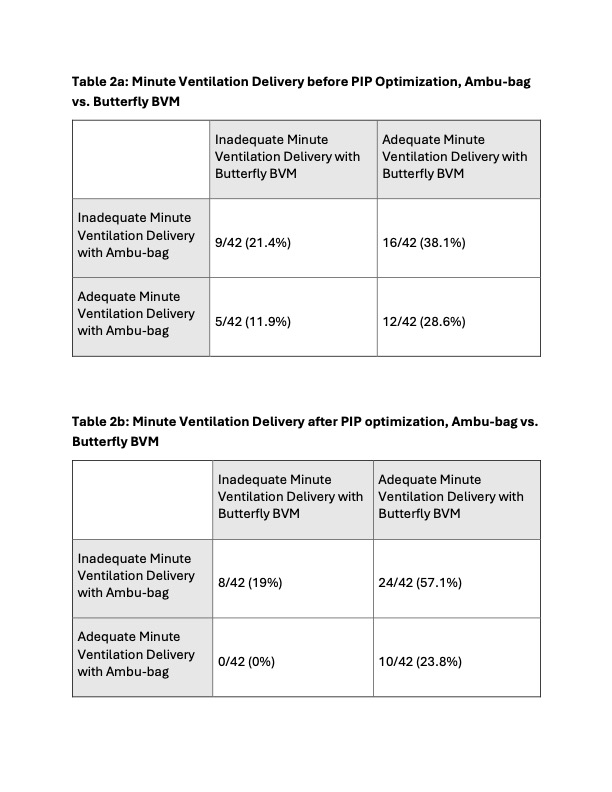 Table 2a: Minute Ventilation Delivery before PIP Optimization, Ambu-bag vs. Butterfly BVM; Table 2b: Minute Ventilation Delivery after PIP optimization, Ambu-bag vs. Butterfly BVM
Table 2a: Minute Ventilation Delivery before PIP Optimization, Ambu-bag vs. Butterfly BVM; Table 2b: Minute Ventilation Delivery after PIP optimization, Ambu-bag vs. Butterfly BVM Table 1
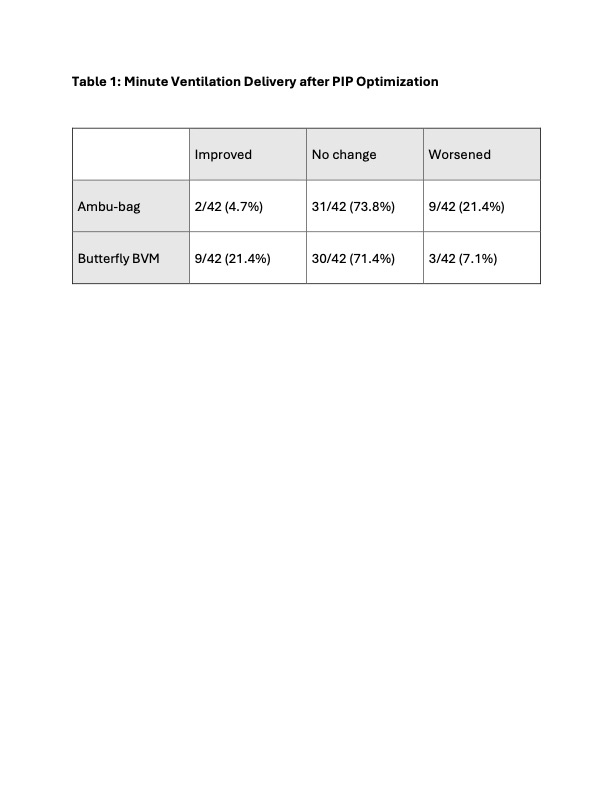 Table 1: Minute Ventilation Delivery after PIP Optimization
Table 1: Minute Ventilation Delivery after PIP Optimization Table 2a and Table 2b
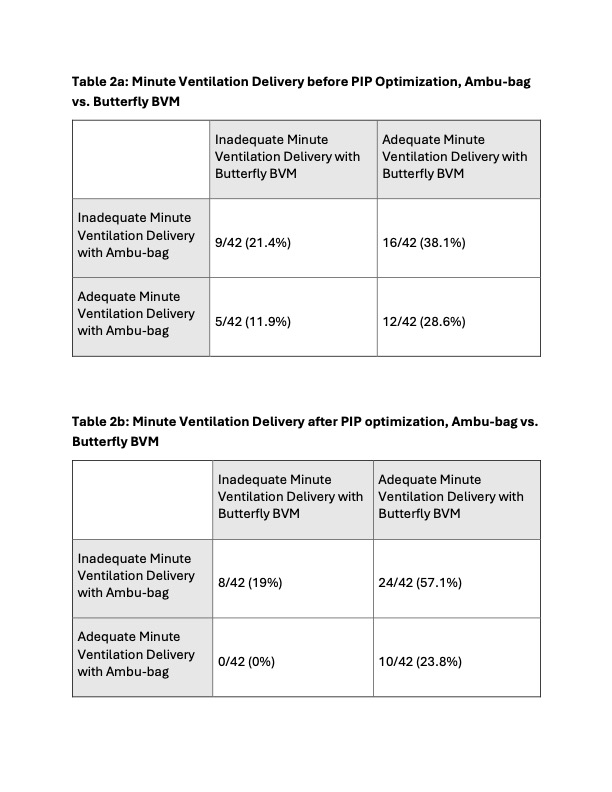 Table 2a: Minute Ventilation Delivery before PIP Optimization, Ambu-bag vs. Butterfly BVM; Table 2b: Minute Ventilation Delivery after PIP optimization, Ambu-bag vs. Butterfly BVM
Table 2a: Minute Ventilation Delivery before PIP Optimization, Ambu-bag vs. Butterfly BVM; Table 2b: Minute Ventilation Delivery after PIP optimization, Ambu-bag vs. Butterfly BVM 
