Medical Education 5: Procedures and Simulation
Session: Medical Education 5: Procedures and Simulation
239 - Reported Barriers to Procedural Experience Among Neonatal-Perinatal Medicine (NPM) Fellows
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 239.6158
Mark R. Castera, Boston University School of Medicine, Boston, MA, United States; Mary T. Crume, University of Texas Southwestern Medical School, Lewisville, TX, United States; Riti Chokshi, University of Texas Southwestern Medical School, Dallas, TX, United States; Bailey Zeiler, Texas Tech University Health Sciences Center School of Medicine, Lubbock, TX, United States; Shoshana Newman-Lindsay, University of California Davis Children's Hospital, Sacramento, CA, United States; Amanda A. Wanous, University of Michigan Medical School, Ann Arbor, MI, United States; Abdul Wasay Khan, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Aashika Janwadkar, John H Stroger Hospital of Cook County, Chicago, IL, United States; Megan Gray, University of Washington School of Medicine, Seattle, WA, United States; Heather M. French, Children's Hospital of Philadelphia, Philadelphia, PA, United States
Mary T. Crume, MD (she/her/hers)
Assistant Professor of Pediatrics
University of Texas Southwestern Medical School, Texas, United States
Presenting Author(s)
Background: NPM fellowship programs need to ensure their fellows attain competency in common and life-saving neonatal procedures prior to graduation into independent practice. There may be fewer opportunities for procedural performance by fellows during training given advances in clinical care and increased numbers of advanced practices providers in the NICU.
Objective: Assess NPM fellows’ perceptions of their procedural experiences and barriers to attaining procedural competency.
Design/Methods: All US NPM fellows were sent a REDCap survey in May 2024 to collect data on their procedural experience in fellowship, and perceptions of and barriers to developing procedural competency. Multiple choice questions were analyzed with descriptive statistics. Qualitative responses underwent general inductive analysis.
Results: 342 NPM fellows completed the survey (39% of 875 fellows) (Table 1). Of the respondents, 81% believe they will have sufficient procedural experience to achieve competency by fellowship graduation (5% disagreed, 14% unsure). More than half of 1st, 2nd, and 3rd year fellows (71%, 67%, and 83% respectively) believe they have had appropriate procedural experience for their level of training. Senior fellows (PGY6) were more likely to report adequate procedural experience than junior fellows (X2 = 17.5, p=0.008) (Figure 1). The most commonly identified barriers to achieving procedural competency were competition with other clinicians (N=170, 50%) and procedural scarcity (N=137, 40%). Many fellows also lament not having opportunities to train in newer procedural techniques such as minimally invasive surfactant therapy and point of care ultrasound due to limitations within their institutions (Table 2).
Conclusion(s): While the majority of NPM fellow participants in this study feel that they will have adequate procedural exposure by graduation needed for competency, 18% of senior fellows believe their procedural experience is below expectations for training. Fellows believe the primary barrier to obtaining appropriate procedural experience is fewer procedures overall coupled with more clinicians competing to perform them. Future studies should explore the impact of policies on procedural allocation amongst clinicians and educational interventions such as simulation.
Table 1
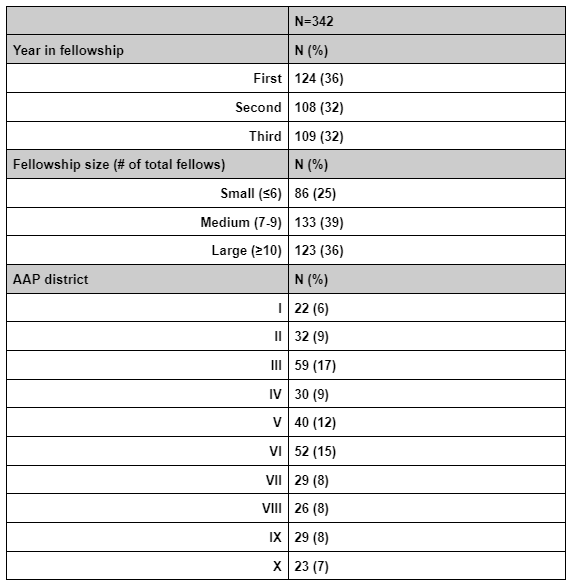 Respondent Trainee Demographics
Respondent Trainee DemographicsFigure 1
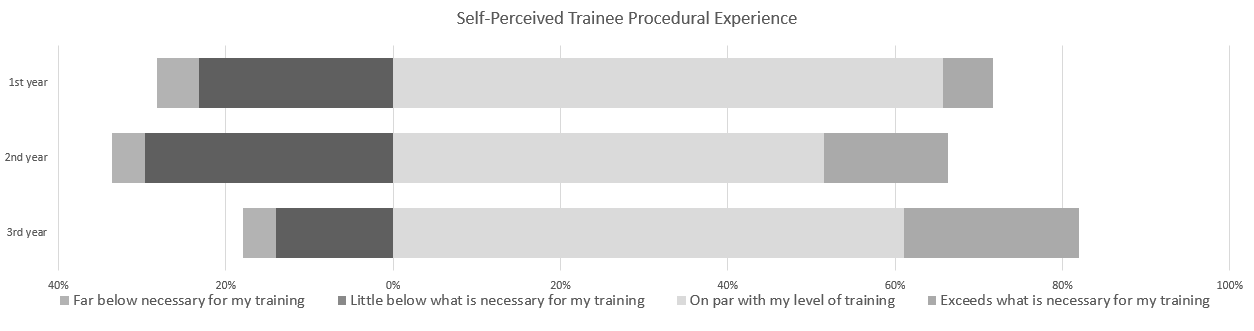 Self-Perceived Trainee Procedural Experience
Self-Perceived Trainee Procedural ExperienceTable 2
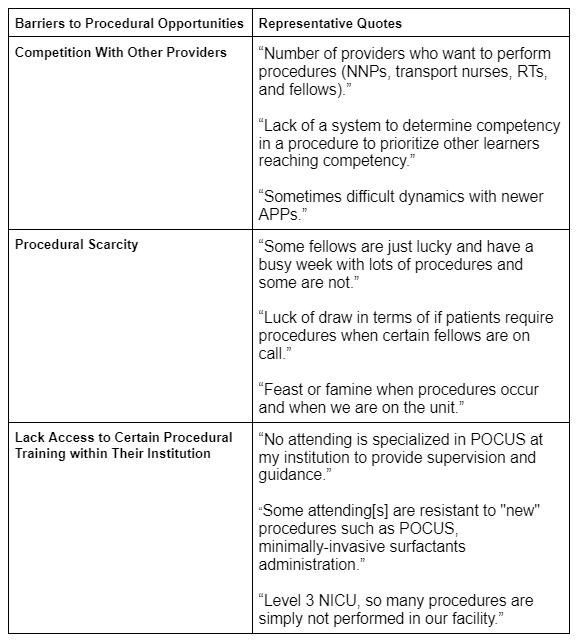 Reported Barriers to Fellow Procedural Opportunities
Reported Barriers to Fellow Procedural OpportunitiesTable 1
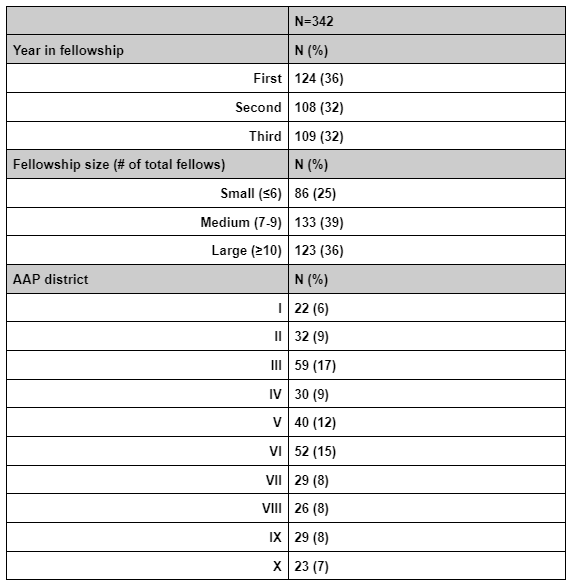 Respondent Trainee Demographics
Respondent Trainee DemographicsFigure 1
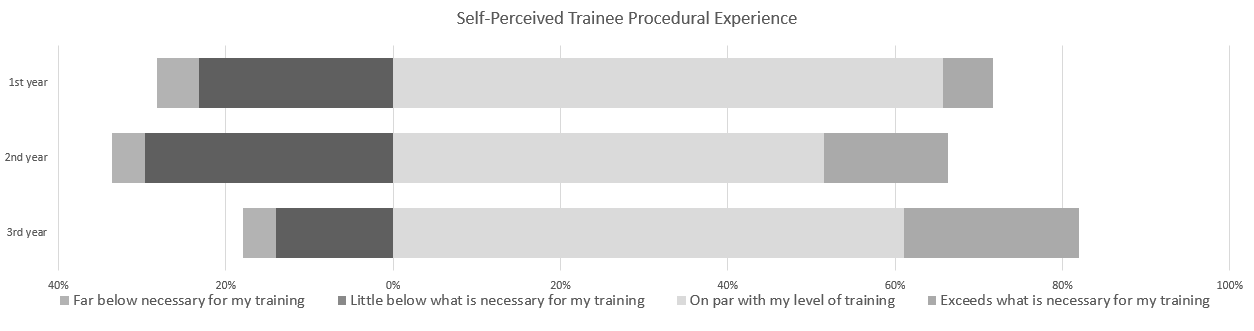 Self-Perceived Trainee Procedural Experience
Self-Perceived Trainee Procedural ExperienceTable 2
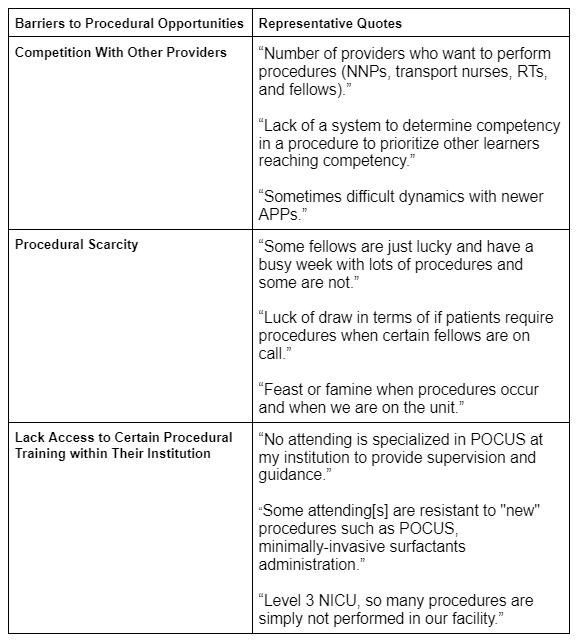 Reported Barriers to Fellow Procedural Opportunities
Reported Barriers to Fellow Procedural Opportunities
