Neonatal Hemodynamics and Cardiovascular Medicine 3
Session: Neonatal Hemodynamics and Cardiovascular Medicine 3
072 - Predicting Respiratory Support at ICU Discharge for Neonates with Symptomatic Congenital Heart Disease
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 72.6321
Mahati Pidaparti, Indiana University School of Medicine, Indianapolis, IN, United States; Britney Reed, Indiana University School of Medicine, Indianapolis, IN, United States; Benjamin M. Helm, Indiana University School of Medicine, Indianapolis, IN, United States; Kristen Suhrie, Indiana University School of Medicine and Riley Children's Health, Indianapolis, IN, United States

Mahati Pidaparti, MD
Fellow
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Many infants with congenital heart disease (CHD) have multiple home health needs after their initial hospitalization, including respiratory support. There are limited studies looking at predictive factors for needing respiratory support needs at discharge (RSND).
Objective: Determine prenatal and early neonatal factors that predict RSND in neonates with CHD.
Design/Methods: A retrospective cohort study was conducted among neonates with CHD who were admitted to a cardiovascular or level IV neonatal intensive care unit (ICU) between January 2021 and December 2023. Maternal demographic and pregnancy data, infant echocardiographic findings, genetic testing results and specifics of initial inpatient stay, including home healthcare needs at discharge, were collected. Bivariate and multivariable logistic regressions were used to quantify the relationships between clinical variables and the outcome of RSND. Prediction models were developed using significant factors and adjusting for interactions between variables and confounders.
Results: Of the 415 patients that met study inclusion criteria, 341 (82%) were discharged home from the ICU, of which 39 infants (11%) had RSND with 23 (7%) needing nasal cannula and 16 (5%) needing tracheostomy (Table 1). While the cardiac lesion type was significantly associated with RSND (p=0.02) in bivariate analysis, it was not significantly associated after multivariable adjustment and accounting for intubation, congenital anomalies, and genetic diagnoses (p=0.19). There were higher odds of RSND with having a genetic diagnosis [OR 2.7 (95% CI: 1.2, 6.5)] and additional major congenital anomalies [4.5 (1.9, 11.7)], while higher birth weight was associated with lower odds [0.5 (0.38, 0.66)]. Using the variables of birth weight, genetic diagnosis, and additional major congenital anomaly, the prediction model of RSND (Figure 1) had a high accuracy of prediction with an area under the curve (AUC) of the receiver-operator characteristic curve (ROC) of 0.86 with 95% CI: (0.79, 0.92) (Figure 2). When adjusting the model for cardiac surgery during the first admission as well as intubation status prior to cardiac surgery, it was even more accurate with AUC improved to 0.89 with 95% CI: (0.82, 0.95) (Figure 2).
Conclusion(s): Cardiac lesion type was not significantly associated with RSND, while birth weight, genetic diagnosis, other anomalies, and intubation course during admission were all significantly associated and highly predictive of RSND. These prediction models can allow clinicians to more precisely counsel families regarding the respiratory outcomes for their child with CHD.
Table 1: Demographic, maternal and neonatal factors of cohort categorized by respiratory support needs at discharge
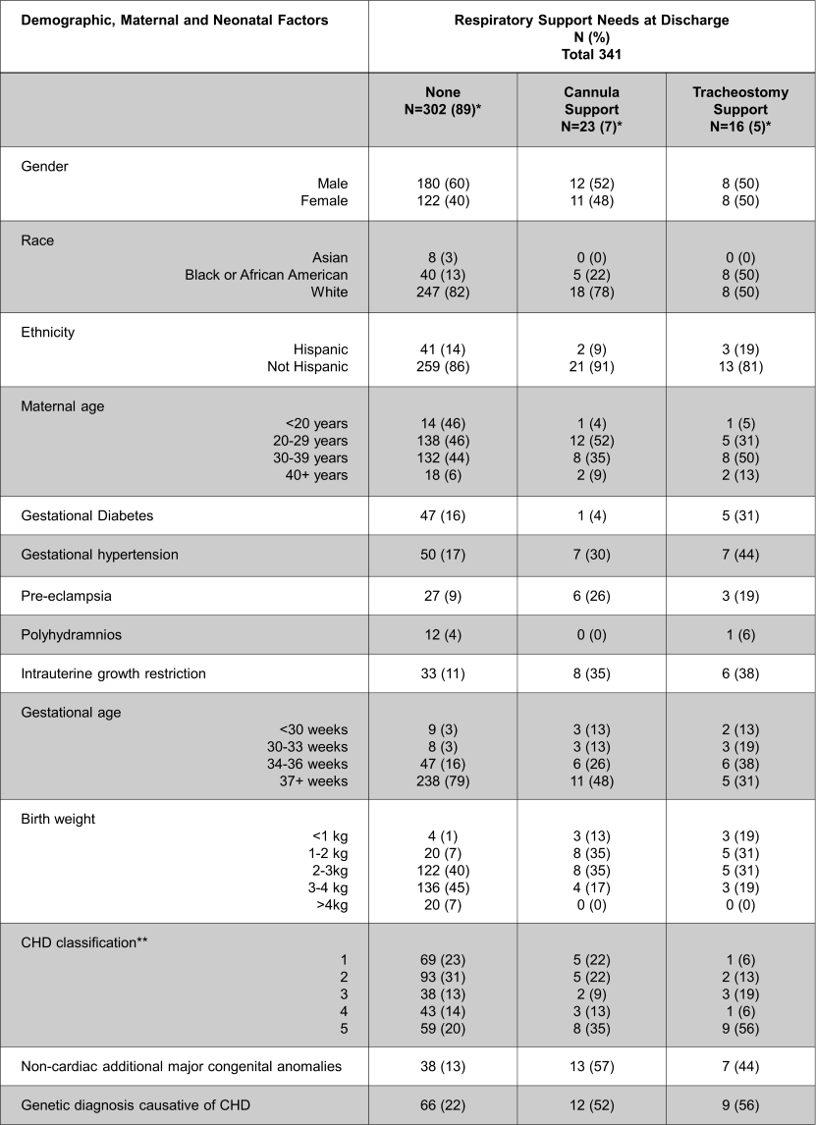 *Percentages may not total to 100 due to missing values.
*Percentages may not total to 100 due to missing values. **CHD Classification system:
1. Cyanotic heart disease with single-ventricle physiology
2. Cyanotic heart disease with two-ventricle physiology and ductal-dependent circulation
3. Cyanotic heart disease with two-ventricle physiology, but not ductal-dependent
4. Acyanotic heart disease, ductal-dependent
5. Acyanotic heart disease, not ductal-dependent
Figure 1: Predicted probabilities of respiratory support
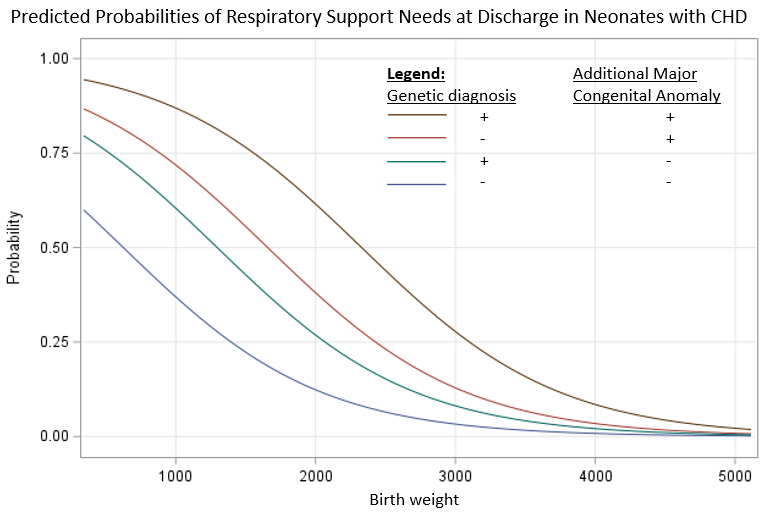 Predicted probabilities of respiratory support at discharge based on birth weight, genetic diagnosis causative of CHD, and additional major congenital anomalies in neonates with symptomatic CHD
Predicted probabilities of respiratory support at discharge based on birth weight, genetic diagnosis causative of CHD, and additional major congenital anomalies in neonates with symptomatic CHDFigure 2: Multivariable logistic regression ROC Curves of Respiratory Support Needs at Discharge in cohort of neonates with symptomatic CHD
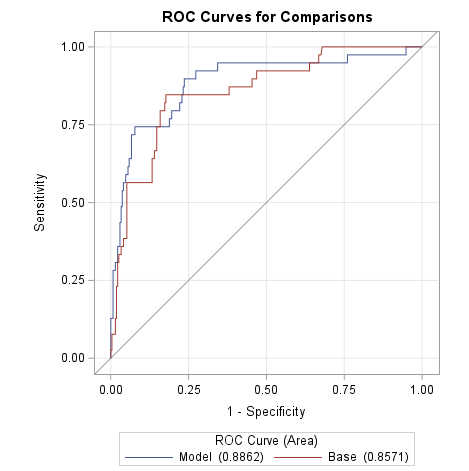 Model 1 using birth weight, genetic diagnosis, and additional major congenital anomaly.
Model 1 using birth weight, genetic diagnosis, and additional major congenital anomaly. Model 2 using birth weight, genetic diagnosis, and additional major congenital anomaly while adjusting for cardiac surgery and intubation status prior to surgery.

