Neonatal Hemodynamics and Cardiovascular Medicine 3
Session: Neonatal Hemodynamics and Cardiovascular Medicine 3
073 - Predicting the Future for Neonates with Symptomatic Congenital Heart Disease
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 73.6320
Mahati Pidaparti, Indiana University School of Medicine, Indianapolis, IN, United States; Benjamin M. Helm, Indiana University School of Medicine, Indianapolis, IN, United States; Britney Reed, Indiana University School of Medicine, Indianapolis, IN, United States; Kristen Suhrie, Indiana University School of Medicine and Riley Children's Health, Indianapolis, IN, United States

Mahati Pidaparti, MD
Fellow
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Congenital heart disease (CHD) is the most common birth defect and contributes significantly to neonatal morbidity and mortality. There is limited understanding of the prenatal and early neonatal factors that predict outcomes for patients with symptomatic CHD in the newborn period.
Objective: Determine prenatal and early neonatal factors that predict infantile outcomes in patients with CHD.
Design/Methods: A retrospective cohort study was conducted among neonates with CHD who were admitted to a cardiovascular or level IV neonatal intensive care unit (ICU) between January 2021 and December 2023. Maternal demographic and pregnancy data, infant genetic reports, echocardiographic findings, and specifics of initial inpatient stay, such as length of stay (LOS) and home healthcare needs at discharge, were collected. Infants’ cardiac lesion types were classified physiologically based on presence or absence of cyanotic lesions, single or double ventricles, and ductal dependence. Statistical analysis was performed using Chi-square and Fisher's Exact Tests for categorical variables and Kruskal-Wallis for continuous variables.
Results: Of the 415 patients that met study inclusion criteria (Table 1), 350 infants (84%) survived to ICU discharge, of which 181 infants (52%) required an enteral feeding tube at discharge. The median length of stay (LOS) for the ICU stay was 36 days (IQR 55). Cardiac lesion type was significantly associated with mortality (p < 0.01), LOS (p < 0.01, and feeding support (p < 0.01) at discharge. Further, having a genetic diagnosis was associated with higher odds of mortality [OR 2.2 (95% CI: 1.3–3.9)] and feeding support [4.4 (2.5–7.9)] at discharge. Likewise, having an additional major congenital anomaly was associated with higher odds of mortality [OR 2.3 (95% CI: 1.2–4.1)] and feeding support [4.8 (2.4–9.7)] at discharge. Finally, a history of polyhydramnios was associated with higher odds of mortality [3.1 (1.2–7.9)], and a history of maternal pre-eclampsia was significantly associated with higher LOS (p < 0.01), but not mortality (p=0.35) or feeding support (p=0.17) at discharge.
Conclusion(s): Of neonates with CHD requiring ICU care in the newborn period, the majority had cyanotic ductal-dependent lesions, and a significant portion had a genetic diagnosis and/or other major congenital anomalies. These 3 factors were found to be critical at predicting mortality, length of stay and ongoing feeding support after discharge.
Table 1: Demographic, maternal and neonatal factors of cohort with bivariate analysis of factors with outcomes of mortality, LOS and enteral feeding support at ICU discharge
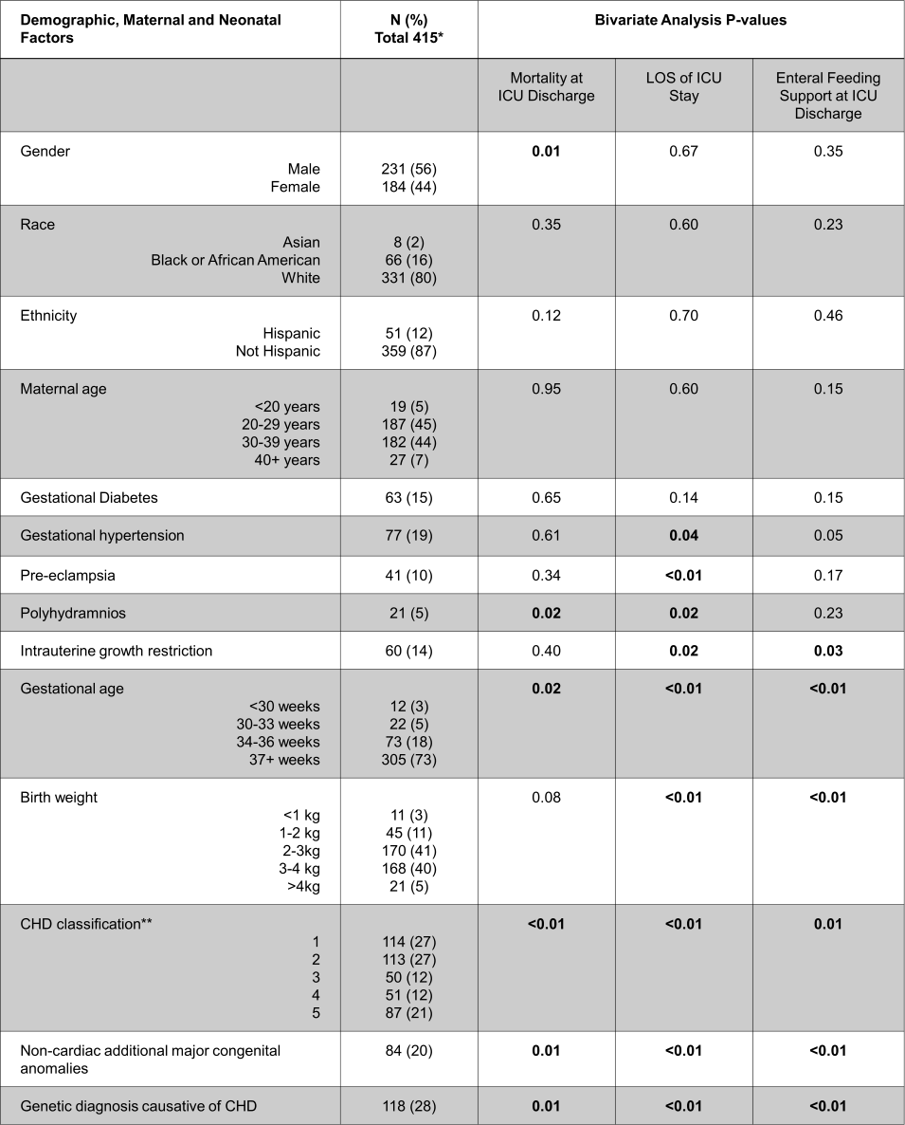 Bivariate analysis was performed using Chi-square and Fisher's Exact Tests for categorical variables (mortality and enteral feeding support at discharge) and Kruskal-Wallis for continuous variables (LOS).
Bivariate analysis was performed using Chi-square and Fisher's Exact Tests for categorical variables (mortality and enteral feeding support at discharge) and Kruskal-Wallis for continuous variables (LOS).*Percentages may not total to 100 due to missing values.
**CHD Classification system:
1. Cyanotic heart disease with single-ventricle physiology
2. Cyanotic heart disease with two-ventricle physiology and ductal-dependent circulation
3. Cyanotic heart disease with two-ventricle physiology, but not ductal-dependent
4. Acyanotic heart disease, ductal-dependent
5. Acyanotic heart disease, not ductal-dependent

