Mental Health 4
Session: Mental Health 4
100 - Mental health conditions among patients with a disorder of the gut-brain interaction
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 100.5980
Ambia S. Ahmed, The Barbara Bush Children's Hospital at Maine Medical Center, South Portland, ME, United States; Nicole Smith, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Anya Cutler, MaineHealth Institute for Research, Montpelier, VT, United States; MariaElena Terzis, The Barbara Bush Children's Hospital at Maine Medical Center, South Portland, ME, United States; Julia Fritz, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Laura J. Faherty, Maine Medical Center/RAND, Cape Elizabeth, ME, United States

Ambia S. Ahmed, MBBS (she/her/hers)
pediatric resident
The Barbara Bush Children's Hospital at Maine Medical Center
South Portland, Maine, United States
Presenting Author(s)
Background: Disorders of the gut-brain interaction (DGBI) are highly prevalent and significantly impact children’s health and well-being. Prior studies have shown that at least 50% of patients with DGBI have co-occurring mood disorders and suggest that anxiety is the most common mental health (MH) comorbidity in DGBI.
Objective: This study aimed to characterize the MH conditions and treatment in patients diagnosed with a DGBI.
Design/Methods: Data were obtained through retrospective chart review of patients in Southern Maine aged 3-18 years who were referred to pediatric gastroenterology between 10/1/2019 and 4/30/2022 and received a DGBI diagnosis. Descriptive statistics were used to understand the population and mental health treatment. Group differences were assessed by Wilcoxon Rank Sum test for continuous variables, and by Chi-Squared and Fisher’s Exact Tests for categorical variables.
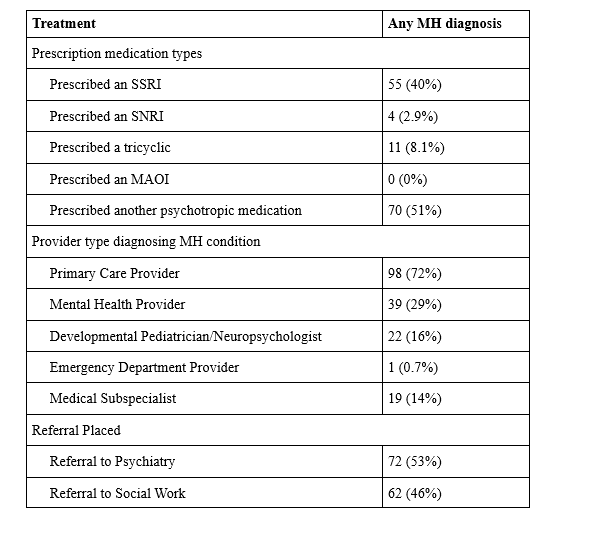
Results: These results reflect data from 185 of 401 charts in the total sample; review is ongoing. Of these 185 patients, 136 (73.5%) had a MH diagnosis in addition to a DGBI diagnosis. Patients who received a MH diagnosis prior to their DGBI diagnosis were older and significantly more likely to have public insurance (Table 1). Roughly equal shares of patients whose MH diagnosis preceded their DGBI diagnosis had public versus private insurance, while nearly two thirds of patients whose MH condition was diagnosed after their DGBI diagnosis were privately insured. Neurodevelopmental and trauma- and stressor-related disorders were more common in patients with a MH diagnosis that preceded their DGBI, while anxiety was more common in those whose DGBI preceded their MH diagnosis (Table 2). Of those with a MH condition, 72% received the diagnosis from their primary care provider. About half of patients with an MH diagnosis were referred to social work or psychiatry (46% and 53%, respectively) (Table 3). There were no significant differences in treatment receipt by timing of MH diagnosis relative to DGBI.
Conclusion(s): MH conditions are common comorbidity among patients with DGBI, highlighting the need for MH assessment and appropriate treatment in patients presenting with DGBI symptoms. There was a difference in insurance when comparing timing of diagnoses. As patients who were diagnosed with a MH condition following DGBI were more likely to have anxiety, the difference in insurance status may be explained by efforts to address somatic symptoms before shifting to MH or secondary to access to resources. A qualitative study of these patients could further elucidate the cause of these differences.
Table 1: Demographic differences between patients with MH diagnosis before their DGBI diagnosis, after their DGBI diagnosis, or No MH diagnosis (Kruskal-Wallis rank sum test; Fisher's exact test; Pearson's Chi-squared test)
.png)
Table 2: Mental Health Diagnoses (N=136)
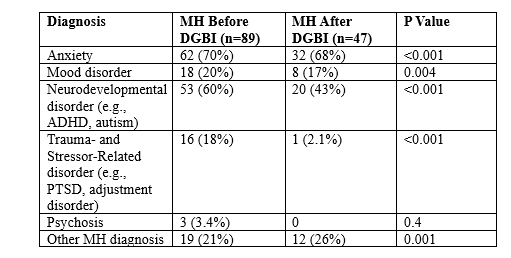
Table 3: Descriptive statistics of documented mental health treatment (n=136)